Machine Learning in Medicine: Real Uses and Benefits
- BLOG
- Artificial Intelligence
- February 16, 2026
Medicine is built on experience, training, and caution. Machine learning in medicine introduces something different: probability-driven insight that improves with data, not years on the ward. That difference creates friction. Models can spot patterns early, yet they can also fail silently if misused or misunderstood.
In response to these realities, this article explores how ML in medicine is applied today. You will learn about real use cases, practical examples, challenges, and what healthcare leaders consider before relying on model-driven decisions that shape safety, trust, and outcomes.
Contents
- 1 What Is Machine Learning in Medicine?
- 2 Why Machine Learning Is Being Adopted in Healthcare
- 2.1 Growing volume and complexity of medical data
- 2.2 Need for earlier risk identification and intervention
- 2.3 Increasing pressure on diagnostic services
- 2.4 Operational strain across hospitals and clinics
- 2.5 Demand for more personalized care decisions
- 2.6 Expectation of measurable performance and accountability
- 3 Build responsible machine learning systems for healthcare.
- 4 Core Medical Areas Where Machine Learning Is Used
- 4.1 Medical imaging and pathology
- 4.2 Risk prediction and early warning in clinical care
- 4.3 Precision medicine and treatment planning
- 4.4 Clinical decision support and workflow support
- 4.5 Remote monitoring and digital health
- 4.6 Medical devices and regulated clinical software
- 4.7 Biomedical research and clinical discovery
- 5 How Machine Learning Works in Medical Settings
- 6 Examples of Machine Learning in Medicine
- 6.1 Autonomous diabetic retinopathy screening in primary care (LumineticsCore previously known as IDx-DR)
- 6.2 Retinal OCT triage and referral suggestions (Moorfields and DeepMind, Nature Medicine study)
- 6.3 Sepsis risk alerts inside the EHR (Epic Sepsis Model external validation)
- 6.4 Atrial fibrillation detection from smartwatch monitoring (Apple Watch study)
- 6.5 AI-enabled medical devices cleared for defined use cases
- 7 Key Challenges of Machine Learning in Medicine
- 8 Machine Learning vs Traditional Clinical Decision Systems
- 9 How Healthcare Organizations Can Adopt Machine Learning Safely
- 9.1 Align machine learning use with clinical responsibility
- 9.2 Limit machine learning to defined medical decisions
- 9.3 Validate machine learning models on local patient populations
- 9.4 Manage bias and fairness in medical predictions
- 9.5 Integrate machine learning into existing clinical workflows
- 9.6 Monitor medical impact after deployment
- 9.7 Control updates to machine learning systems used in care
- 10 How Webisoft Supports Machine Learning in Medicine
- 11 Build responsible machine learning systems for healthcare.
- 12 Conclusion
- 13 Frequently Asked Question
What Is Machine Learning in Medicine?
Machine learning in medicine uses data driven algorithms to detect patterns in medical data and support clinical and operational healthcare decisions across healthcare systems. Unlike traditional clinical systems that rely on fixed rules, machine learning models improve by learning from examples.
Thus making them suitable for complex medical scenarios where relationships are not easily defined in advance. In healthcare settings, these models are trained on data such as electronic health records, medical images, laboratory results, genomic data, and clinical notes.
Once trained, they can assist with tasks like predicting patient risk, supporting diagnosis, prioritizing cases, or estimating treatment outcomes. Importantly, ML in medicine is designed to support clinicians rather than replace them, requiring careful validation, oversight, and alignment with real clinical workflows.
Why Machine Learning Is Being Adopted in Healthcare
 Healthcare systems handle growing data volumes, complex cases, and time-sensitive decisions every day. Machine learning is adopted to support clinicians with pattern recognition and prediction where manual review becomes impractical. It addresses scale, consistency, and early risk identification.
Healthcare systems handle growing data volumes, complex cases, and time-sensitive decisions every day. Machine learning is adopted to support clinicians with pattern recognition and prediction where manual review becomes impractical. It addresses scale, consistency, and early risk identification.
Growing volume and complexity of medical data
Electronic records, imaging, lab results, and monitoring devices generate more data than clinicians can review during routine care. Machine learning helps process large datasets and surface clinically relevant signals without adding cognitive load.
Need for earlier risk identification and intervention
Many clinical conditions worsen before symptoms are obvious. Predictive models can identify risk patterns earlier, supporting timely clinical review and preventive action.
Increasing pressure on diagnostic services
Radiology and pathology workloads continue to rise while staffing remains limited. Machine learning supports prioritization and detection tasks to manage volume and reduce delays.
Operational strain across hospitals and clinics
Healthcare organizations face staffing shortages, scheduling challenges, and resource constraints. Machine learning assists with triage, capacity planning, and workflow support when aligned with clinical operations.
Demand for more personalized care decisions
Standard treatment protocols do not reflect patient variability. Machine learning models analyze multiple patient factors to support individualized risk and treatment considerations.
Expectation of measurable performance and accountability
Healthcare leaders require tools that show validated performance and known limitations. Adoption favors systems with clear evaluation, monitoring, and governance processes.
Build responsible machine learning systems for healthcare.
Discuss clinical use cases, validation needs, and deployment considerations with Webisoft.
Core Medical Areas Where Machine Learning Is Used
 Hospitals use machine learning where data is dense and decisions are time-sensitive. The applications of machine learning in medicine usually cluster around imaging, prediction, personalization, workflow support and medical research. Each area succeeds best when outputs fit how clinicians work and document care.
Hospitals use machine learning where data is dense and decisions are time-sensitive. The applications of machine learning in medicine usually cluster around imaging, prediction, personalization, workflow support and medical research. Each area succeeds best when outputs fit how clinicians work and document care.
Medical imaging and pathology
Machine learning is widely used with images because scans and slides are structured, high-volume inputs. Systems can flag findings, quantify structures, and help sort worklists, so clinicians review the highest-risk cases first. Common uses:
- Detecting abnormalities on X-ray, CT, MRI, and ultrasound
- Segmenting tumors, organs, or lesions for measurement
- Prioritizing urgent studies in radiology queues
- Assisting digital pathology review of slides
Risk prediction and early warning in clinical care
These models analyze patterns across vitals, labs, diagnoses, and medication history to estimate risk. They are used for earlier alerts, triage support, and planning follow-up care, especially when deterioration can happen quickly. Common uses:
- Predicting clinical deterioration or ICU transfer risk
- Readmission risk scoring for discharge planning
- Sepsis or adverse event risk flags as decision support
- Population risk stratification for chronic disease programs
Precision medicine and treatment planning
Machine learning supports personalized decisions by combining patient factors that do not fit one rule set. This includes patient stratification, prognosis estimation, and treatment response signals, often using genomic and phenotypic inputs. Common uses:
- Patient subgrouping for targeted therapies
- Predicting treatment response or side-effect risk
- Prognosis modeling using multi-factor histories
- Supporting therapy selection in oncology and complex care
Clinical decision support and workflow support
Many deployments aim at reducing friction in day-to-day care rather than making final decisions. Examples include supporting documentation, surfacing relevant prior history, and helping leaders assess model limits during training, validation, and deployment. Common uses:
- Triage support and care pathway suggestions
- Documentation support from structured and unstructured inputs
- Case prioritization using risk scores and clinical rules
- Monitoring model behavior when workflows or data change
Remote monitoring and digital health
Wearables and home devices create continuous streams of signals. Machine learning helps interpret trends, reduce noise, and flag events that may need clinical review, especially for chronic conditions and post-discharge monitoring. Common uses:
- Detecting abnormal trends in heart rate, sleep, or activity
- Predicting flare-ups or relapse risk in chronic disease
- Identifying adherence or monitoring gaps
- Triggering clinician review based on risk thresholds
Medical devices and regulated clinical software
A growing number of AI-enabled medical devices are authorized for marketing, which reflects real clinical usage in specific specialties. In regulated contexts, machine learning is packaged as software within devices or clinical tools with defined indications and controls. Common uses:
- Device software that assists image analysis or measurement
- Specialty-focused clinical tools with validated indications
- Tools designed with post-market monitoring expectations
- Systems that require clear labeling of intended use
Biomedical research and clinical discovery
Beyond direct patient care, machine learning plays a significant role in medical research. It helps researchers analyze large datasets, identify hidden patterns, and generate hypotheses that would be difficult to detect manually. Common uses:
- Analyzing genomic and proteomic datasets
- Identifying potential drug targets
- Optimizing clinical trial recruitment and design
- Detecting novel disease subtypes from large patient datasets
How Machine Learning Works in Medical Settings
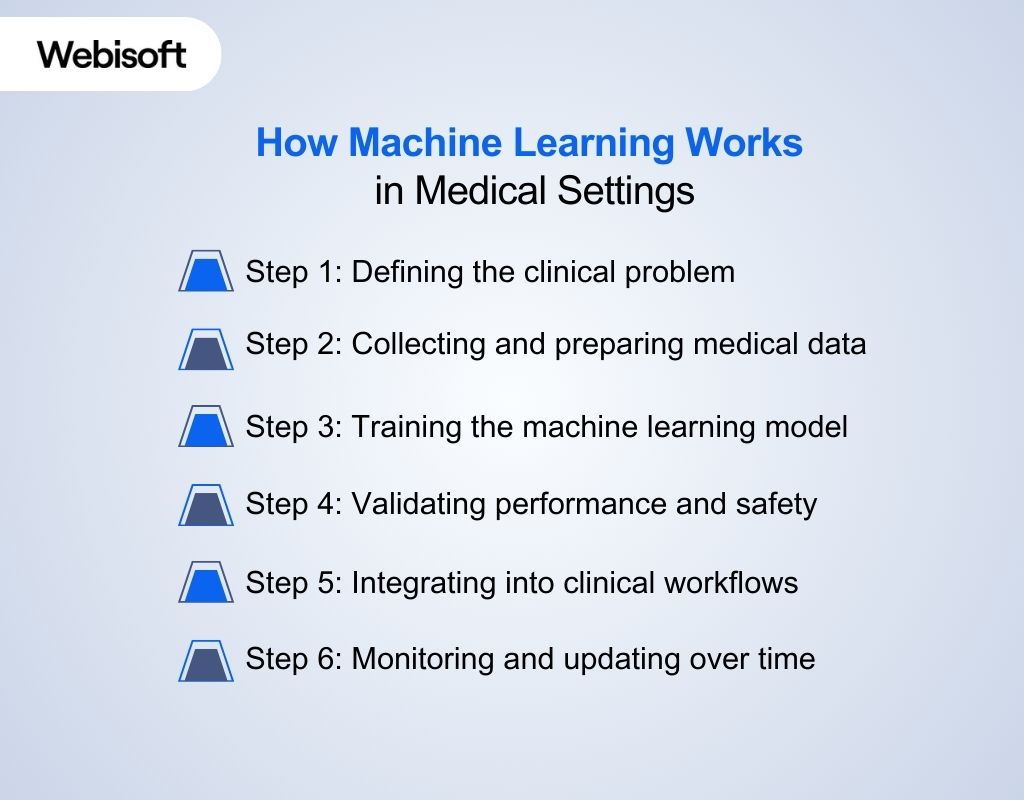 In medical settings, machine learning follows a structured process that moves from clinical need to real-world use. Each step focuses on safety, data quality, and workflow alignment. The goal is reliable support, not autonomous decision-making.
In medical settings, machine learning follows a structured process that moves from clinical need to real-world use. Each step focuses on safety, data quality, and workflow alignment. The goal is reliable support, not autonomous decision-making.
Step 1: Defining the clinical problem
The process begins by identifying a specific clinical or operational problem where a prediction or classification can support care. Teams define who will use the output, when it appears, and how it influences decisions. Clear success criteria are set before any model work starts.
Step 2: Collecting and preparing medical data
Relevant data is gathered from sources such as electronic health records, imaging systems, laboratories, and monitoring devices. Preparation includes cleaning records, handling missing values, aligning timelines, and confirming that data reflects real clinical practice without leakage or bias.
Step 3: Training the machine learning model
The model is trained using historical data so it can learn relationships between inputs and outcomes. The choice of method depends on the data type and task, such as tabular records or images. Training includes comparing results against existing clinical approaches.
Step 4: Validating performance and safety
Before clinical use, models are tested on data they have not seen before. Validation checks accuracy, calibration, and failure cases. Clinical teams review errors to understand where predictions may mislead or require caution.
Step 5: Integrating into clinical workflows
Deployment focuses on placing outputs inside existing systems, often through electronic health records. The timing and presentation of results are adjusted so clinicians can interpret them quickly without disrupting routine care.
Step 6: Monitoring and updating over time
After deployment, performance is tracked continuously as data and practice patterns change. Models may require recalibration or retraining, along with governance processes that address safety, accountability, and regulatory expectations.
Examples of Machine Learning in Medicine
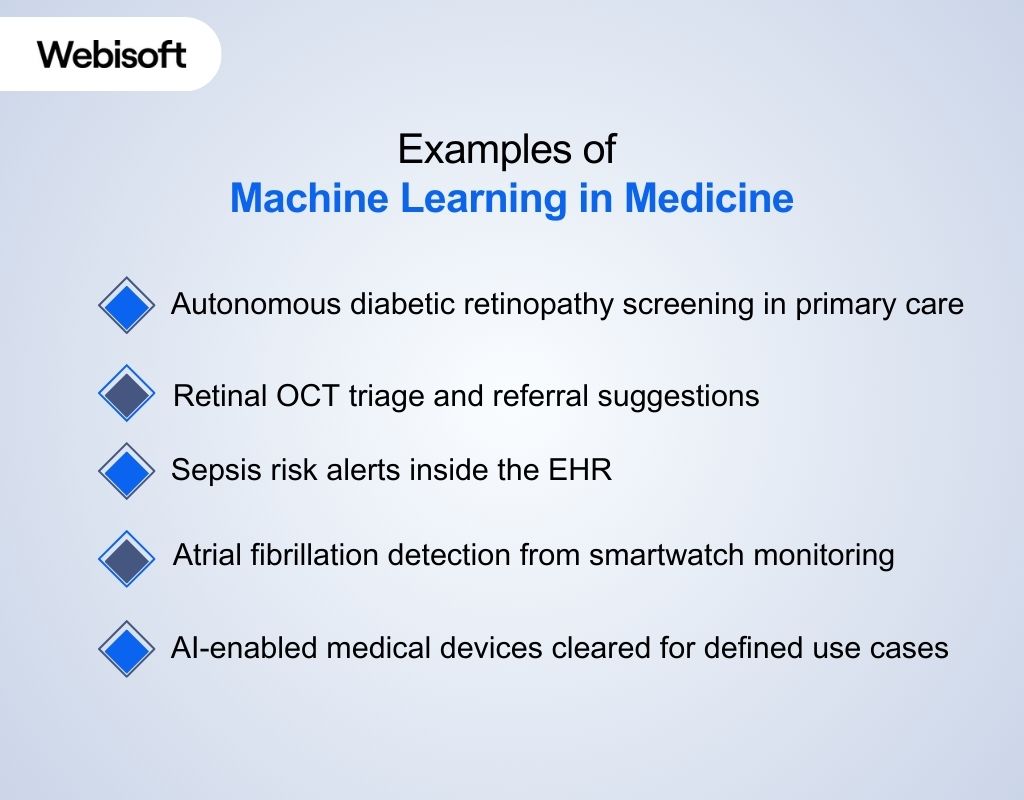 If you search for machine learning in medicine examples, you will mostly see systems that already touch clinical care, not lab demos. The best-known examples fall into screening, imaging support, hospital risk alerts, and wearable-based monitoring, with clear boundaries on what the model can claim.
If you search for machine learning in medicine examples, you will mostly see systems that already touch clinical care, not lab demos. The best-known examples fall into screening, imaging support, hospital risk alerts, and wearable-based monitoring, with clear boundaries on what the model can claim.
Autonomous diabetic retinopathy screening in primary care (LumineticsCore previously known as IDx-DR)
The FDA authorized an AI system that can detect “more than mild” diabetic retinopathy from retinal images and return a clear refer-or-rescreen result. It is designed for use by healthcare providers and supports screening access outside specialist eye clinics.
Retinal OCT triage and referral suggestions (Moorfields and DeepMind, Nature Medicine study)
A widely cited example in ophthalmology uses deep learning on OCT scans to help classify retinal disease and recommend referral urgency. The work is often referenced because it pairs model output with a workflow action, not just a probability score.
Sepsis risk alerts inside the EHR (Epic Sepsis Model external validation)
Sepsis prediction tools are deployed in hospital EHR environments to warn clinicians when a patient may be developing sepsis. Independent validation of the Epic Sepsis Model showed lower sensitivity and precision than reported, producing many false positives and missing numerous true sepsis cases. This made it a real-world example of why local testing matters before relying on an alert.
Atrial fibrillation detection from smartwatch monitoring (Apple Watch study)
Wearables have become a large-scale setting for ML-driven detection. A major Apple Watch study reported that irregular rhythm notifications aligned with ECG patch findings for many participants. Thus showing how consumer devices can support earlier signal detection at population scale.
AI-enabled medical devices cleared for defined use cases
Beyond headline examples, the FDA has a growing set of AI-enabled devices, especially in imaging-adjacent categories, with defined intended use and labeling. This matters because it reflects where machine learning is packaged into regulated tools rather than experimental prototypes.
Real-world deployments show that success depends as much on execution as on models. Webisoft helps healthcare teams build machine learning systems that work in real clinical environments by translating clinical intent into dependable, production-ready solutions.
Key Challenges of Machine Learning in Medicine
Machine learning tools can look strong in development yet disappoint in daily clinical use. The gaps usually come from data quality, validation limits, workflow friction, and governance. These challenges matter because errors can affect patient safety and clinician trust.
- Messy clinical data: EHR data is incomplete, inconsistent, and shaped by billing and documentation habits, which can mislead models trained on it.
- Hidden bias and unequal performance: Models can perform differently across populations due to skewed training data, proxy variables, and missingness patterns, raising fairness and safety concerns.
- Data leakage during development: When training uses information that would not be available at prediction time, results look better than reality and fail after deployment.
- Weak external validation: A model that works in one hospital or time period may not transfer to another, which is why independent testing is essential.
- Poor calibration at the bedside: Even with decent ranking metrics, risk scores can be miscalibrated, leading to overreaction or missed urgency if thresholds are wrong for local practice.
- Workflow mismatch and alert fatigue: If outputs arrive at the wrong time, in the wrong place, or too frequently, clinicians ignore them, which can reduce safety and adoption.
- Model drift after deployment: Changes in patient mix, clinical practice, coding, or EHR configuration can degrade performance over time, requiring monitoring and controlled updates.
- Regulatory and quality controls: In regulated contexts, teams need documented development practices, risk controls, and change management for updates, not just a one-time model release.
- Steep learning curve for clinical teams: Clinicians and operational staff must understand what a model does, its limits, and how to interpret outputs. Without training and alignment, even well-performing systems may be underused or misapplied.
- Publications and dissemination gaps: Research findings often highlight model performance under controlled conditions, but published results may not fully reflect real-world deployment complexity. Limited transparency around methods and datasets can hinder reproducibility and trust.
- Limited explainability in complex models: Many machine learning systems, especially deep learning models, operate as black boxes. When clinicians cannot understand why a prediction was made, trust decreases and adoption slows, particularly in high-risk decisions.
Machine Learning vs Traditional Clinical Decision Systems
Healthcare teams rely on both rule-based tools and machine learning systems to support decisions. These approaches differ in how they process data, handle uncertainty, and scale across care settings. Understanding their differences helps reduce risk and set realistic expectations.
| Comparison area | Traditional clinical decision systems | Machine learning systems |
| Decision logic | Uses predefined if-then rules based on guidelines and protocols. | Learn patterns from historical data to generate predictions or scores. |
| Best suited problems | Stable, well-defined rules such as drug interactions or protocol reminders. | Complex pattern recognition such as imaging support or risk prediction. |
| Data dependency | Limited data needed since logic is manually defined. | Requires large, representative datasets for training and validation. |
| Transparency | Easy to interpret because each output maps to a known rule. | Often less interpretable, requiring validation and monitoring for trust. |
| Validation focus | Ensures rules fire correctly under expected conditions. | Tests generalization, calibration, bias, and failure cases. |
| Common risks | Outdated rules, incorrect mappings, missed triggers. | Overfitting, data leakage, poor transfer across hospitals. |
| Maintenance needs | Manual updates when guidelines or workflows change. | Ongoing monitoring and controlled updates as data and practice evolve. |
| Typical use in practice | Policy-driven alerts and standardized care pathways. | Prediction and prioritization, often paired with clinical rules. |
How Healthcare Organizations Can Adopt Machine Learning Safely
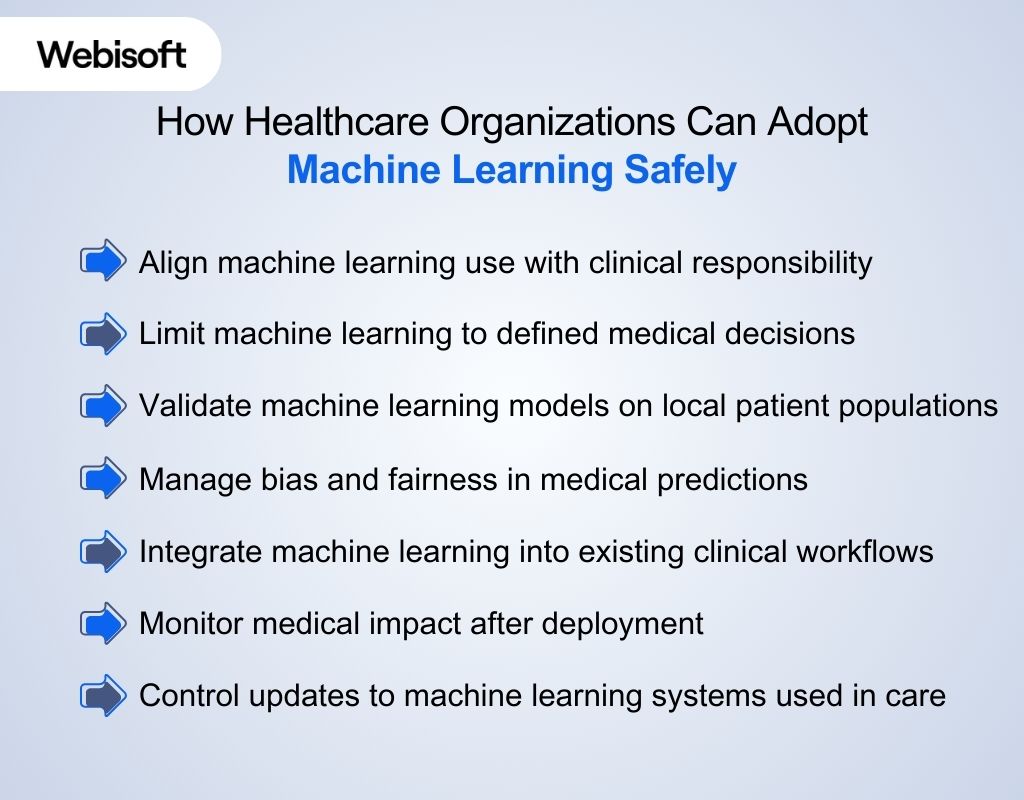 Adopting AI and machine learning in medicine requires more than technical capability. Healthcare organizations must align clinical responsibility, patient safety, and regulatory expectations with how models influence medical decisions. Safe adoption depends on structure, limits, and oversight within medical practice.
Adopting AI and machine learning in medicine requires more than technical capability. Healthcare organizations must align clinical responsibility, patient safety, and regulatory expectations with how models influence medical decisions. Safe adoption depends on structure, limits, and oversight within medical practice.
Align machine learning use with clinical responsibility
ML in medicine must operate under clear clinical responsibility. Organizations need to decide which medical roles review outputs, override recommendations, and remain accountable for patient outcomes.
Limit machine learning to defined medical decisions
Safe adoption requires restricting models to specific medical decisions such as risk signaling, prioritization, or screening support. Open-ended or ambiguous use increases patient safety and liability risks.
Validate machine learning models on local patient populations
Medical data varies across hospitals, regions, and specialties. Models must be evaluated on local patient populations to ensure predictions remain relevant and clinically safe.
Manage bias and fairness in medical predictions
Healthcare organizations must assess whether machine learning systems perform unevenly across age, sex, ethnicity, or clinical subgroups. Bias in medical predictions can worsen health disparities if left unchecked.
Integrate machine learning into existing clinical workflows
Machine learning outputs should support existing medical workflows rather than change how clinicians practice medicine. Poor integration leads to alert fatigue and ignored recommendations.
Monitor medical impact after deployment
Once in use, machine learning systems must be monitored for changes in accuracy, behavior, and unintended clinical effects. Ongoing review protects patient safety as care patterns evolve.
Control updates to machine learning systems used in care
Any change to a model used in medical decision support can affect outcomes. Organizations must review, test, and document updates before they influence patient care.
How Webisoft Supports Machine Learning in Medicine
 When machine learning moves into patient care, you need more than a model. You need a partner who can ship reliable systems, keep them stable in production, and support clinical teams with clear limits and oversight. That is where Webisoft fits.
When machine learning moves into patient care, you need more than a model. You need a partner who can ship reliable systems, keep them stable in production, and support clinical teams with clear limits and oversight. That is where Webisoft fits.
From clinical ideas to ML roadmaps
We work with you to translate clinical goals into realistic machine learning initiatives. Our team helps define the right use cases, success metrics, and boundaries so projects stay focused on outcomes that matter in medical settings.
Medical-grade model development
Our engineers build machine learning models around your actual healthcare data, not generic assumptions. We focus on accuracy, validation, and reliability so models can support real clinical and operational decisions.
Production-ready ML delivery
We specialize in taking machine learning beyond pilots. Our work includes building stable data pipelines, deployment support, and integration planning, so models function reliably in live healthcare environments.
Drift monitoring and model stability
Medical data changes over time. We help you monitor performance, detect drift, and manage updates so models continue to behave as expected after deployment, without introducing hidden risks.
AI-enabled healthcare products
When machine learning is part of a broader healthcare product, we support the full system. Our experience in healthcare software development allows us to deliver AI-enabled platforms that work end to end.
A true extension of your team
We work closely with your clinicians, engineers, and leaders throughout the project. Clear communication, shared ownership, and practical documentation help keep everyone aligned as your machine learning systems continue operating in real clinical environments.
You’ve already seen how these systems are planned, built, and supported in real healthcare environments. Continue the conversation through the Webisoft contact page to discuss your specific medical use case, data constraints, and expectations around safety, validation, and long-term support.
Build responsible machine learning systems for healthcare.
Discuss clinical use cases, validation needs, and deployment considerations with Webisoft.
Conclusion
At this point, it is clear that machine learning in medicine is not a future concept. It already influences how risks are surfaced, decisions are supported, and care is prioritized, with outcomes depending heavily on how responsibly it is applied.
That responsibility ultimately comes down to execution. Teams ready to move forward can work with Webisoft to apply machine learning that respects data, clinical workflows, and accountability without compromising patient care.
Frequently Asked Question
Can machine learning improve disease diagnosis?
Yes. Machine learning models analyze imaging, laboratory results, and clinical records to identify patterns that may be missed during manual review. When properly validated, they can support earlier detection and more consistent diagnosis in high volume clinical environments.
Is machine learning replacing doctors?
No. Machine learning supports clinicians by providing risk estimates, pattern recognition, and decision signals. Medical judgment, treatment decisions, and responsibility for patient outcomes remain with licensed healthcare professionals at all times.
How accurate are machine learning models in healthcare?
It depends. Accuracy varies by clinical task, data quality, and validation rigor. Some models outperform traditional methods in specific use cases, but all require local testing, monitoring, and clinical oversight before use in patient care.