Over recent years, there’s been a noticeable uptick in healthcare data issues. These problems often stem from mishandling. And also for not disposing of data correctly, and unauthorized sharing.
To address these challenges, it’s essential to turn to solutions that align with established guidelines.
And the key lies in HIPAA compliant software development. To tackle these challenges, it’s essential to have software like this. Then, let’s understand what being HIPAA compliant really means and how it works.
Contents
- 1 WHat is HIPAA?
- 2 Definition of HIPAA-Compliant Software
- 3 Key Features for Software Aligned with HIPAA
- 4 Achieving HIPAA Compliance: Step by Step Process
- 5 How to Build HIPAA Compliant Software on AWS Cloud?
- 6 The Imperative of HIPAA Compliance
- 7 What are the Need for HIPAA Compliance in Healthcare Apps?
- 8 HIPAA Compliant Software Development in Webisoft
- 9 Conclusion
- 10 FAQS
WHat is HIPAA?
HIPAA, or the “Health Insurance Portability and Accountability Act,” is a crucial federal regulation. Its main goal is to ensure that patient health details remain private unless the individual gives permission for its release.
This law led the US Department of Health and Human Services to introduce specific rules to safeguard what’s known as Protected Health Information or PHI.
Now, if your business handles PHI or its electronic version, ePHI, you need to align your systems with HIPAA’s standards. This isn’t just for healthcare providers who offer treatments or handle payments.
Even if you’re a business partner with access to details about patients, their treatments, or payments, you’re on the hook to stay HIPAA compliant.
Definition of HIPAA-Compliant Software
When we talk about software that’s in line with HIPAA, we’re referring to tools or services designed for healthcare organizations.
These tools come equipped with the necessary measures to ensure both privacy and security, in line with HIPAA standards. Some of these tools might focus on specific aspects of the HIPAA guidelines. While others provide a comprehensive solution covering all areas.
The main goal behind creating such software is to give those in charge of compliance a reliable structure. This ensures they’re ticking all the boxes. Such as from security to privacy, and from breach alerts to other essential rules.
Key Features for Software Aligned with HIPAA
Let’s find out the key features of this software:
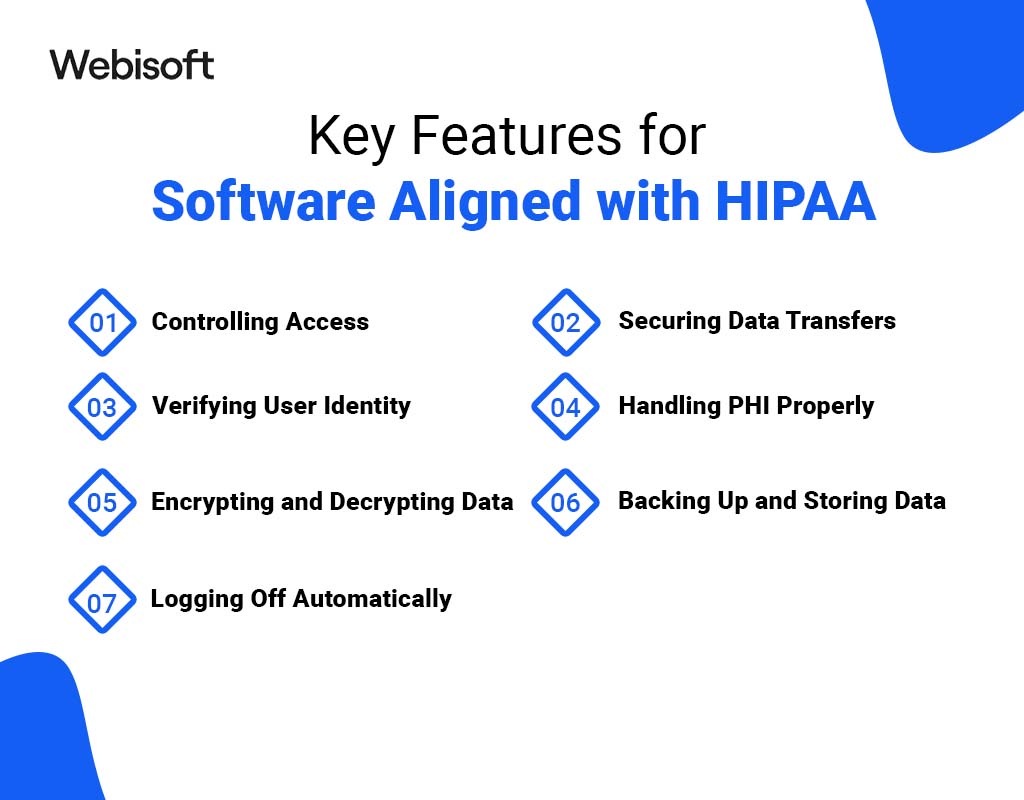
Controlling Access
Software that holds sensitive patient data needs to be particular about who gets to see or change that information.
According to HIPAA for software developers, guidelines are, only the necessary amount of patient data should be visible to any user. This means giving each user a unique identifier. By doing this, you can track and oversee the actions of individuals using your system.
For instance, while a doctor might have the right to read, write, and update a patient’s medical record, a lab assistant might only be allowed to make updates.
Securing Data Transfers
When you’re sending patient data across networks or between different parts of your system, it’s crucial to keep that information safe. This is where HTTPS comes into play.
It’s a protocol that encrypts data using methods like TLS/SSL. When a browser connects to your system, it asks for a certificate.
After verifying its authenticity, an encrypted connection is established. If you’re thinking of transferring files with patient data, consider using protocols like FTPS or SSH instead of the standard FTP.
Verifying User Identity
Once you’ve set user permissions, you need to be sure that the person trying to access the data is who they say they are. There are several ways to do this:
- Using a password
- Relying on biometric data
- Utilizing a personal identification number
- Employing physical identification methods
Remember, passwords might seem straightforward, but they can also be vulnerable. Many security incidents occur because of stolen or easily guessed passwords.
Think about combining a strong password with another verification method, like a one-time password sent via text.
Handling PHI Properly
It’s not just about storing patient data. Also, it’s about getting rid of it responsibly when it’s no longer needed. Just deleting data isn’t enough if a copy remains in a backup somewhere.
A notable incident involved Affinity Health Plan. It’s returned photocopiers without wiping their hard drives, leading to a significant data breach. PHI can be found in unexpected places, from scanners to SD cards.
Thus, when you’re disposing of data, ensure you also destroy any devices or media that held it.
Encrypting and Decrypting Data
One of the best ways to keep PHI safe is through encryption. Without the right decryption keys Even if someone manages to get their hands on the data, it’s meaningless.
Especially with devices like laptops or phones, encryption can prevent many potential breaches.
Backing Up and Storing Data
Having backups is essential. Unexpected events, from server failures to natural disasters, can compromise your data.
So, it’s wise to have multiple copies of your data in different places.
But remember, a backup is only as good as its restore process. Regularly test your backups to make sure they work. And, of course, these backups should also meet HIPAA’s security standards.
Logging Off Automatically
Any system containing patient data should log users out after a period of inactivity. This simple step can protect data if someone leaves a device unattended.
The exact time can vary based on the platform and environment. For instance, a desktop in a secure location might have a longer timer than a mobile app.
While these features are essential for HIPAA compliance, they alone won’t ensure complete security. However, they can demonstrate to auditors that you’re taking the necessary steps to safeguard client information.
Achieving HIPAA Compliance: Step by Step Process
Becoming HIPAA compliant involves a series of steps tailored to healthcare organizations:

1. Develop Clear Security and Privacy Policies
Becoming HIPAA compliant requires more than just adhering to rules. It involves proactive steps.
One crucial step is creating and maintaining security and privacy policies. These policies should be well-documented, regularly updated, and communicated to staff.
Employees must undergo HIPAA training at least once a year. They should confirm their understanding of these policies.
Healthcare organizations are also obligated to provide patients with a Notice of Privacy Practices (NPP), outlining their rights concerning their medical records.
2. Appoint a Security and Privacy Officer
Navigating the complex world of HIPAA requires in-house experts. The HIPAA Security Rule mandates the appointment of a privacy compliance officer. He’s responsible for policy development and enforcement.
Large organizations are encouraged to form a privacy oversight committee to assist with policy creation and oversight. Regular training for these officers and committee members keeps them up-to-date with evolving HIPAA regulations.
3. Conduct Regular Risk Assessments and Self-Audits
HIPAA compliance isn’t a one-and-done deal. The Department of Health and Human Services (HHS) requires periodic audits and self-assessments. It consists of administrative, physical, and technical safeguards.
Any compliance gaps discovered should be addressed with written remediation plans, outlining how and when violations will be rectified.
4. Implement Security Safeguards
To safeguard electronic protected health information (ePHI), HIPAA’s Security Rule demands three types of safeguards:
- Technical Safeguards: Access control, encryption for data in transit and at rest, audit controls, and integrity controls.
- Physical Safeguards: Control over access to facilities where ePHI is stored, as well as security measures for devices and workstations.
- Administrative Safeguards: Designation of security personnel, implementation of information access management systems, documentation of security management processes, regular security protocol assessments, and workforce security training.
5. Establish a Breach Notification Protocol
Mistakes can happen, but failing to report them can lead to trouble. The HIPAA Breach Notification Rule mandates organizations to report breaches to the OCR and notify affected patients.
It’s essential to have a documented breach notification process outlining compliance with this rule.
6. Document Everything
Comprehensive documentation is key. Record all HIPAA compliance activities, including security and privacy policies, self-audits, risk assessments, staff training, and remediation plans.
This documentation is subject to review during complaint investigations and audits by the Office for Civil Rights (OCR).
How to Build HIPAA Compliant Software on AWS Cloud?
In today’s world, businesses are increasingly turning to cloud providers. Such as Amazon Web Services (AWS) to streamline their operations and manage their IT infrastructure.
This trend extends to healthcare providers who are now leveraging the AWS cloud. They handle, process, and share Protected Health Information (PHI).
Also, they adhere to the regulations laid out in the Health Insurance Portability and Accountability Act (HIPAA).
AWS offers a comprehensive range of HIPAA-compliant services. It makes it possible to develop secure, scalable, and resilient solutions tailored to various healthcare needs.
In the context of developing HIPAA-compliant software, it’s essential to consider the some primary tiers that make up the software architecture:
1. Client Interface
This is the part of the software that users interact with directly. Whether it’s a web application, a mobile app, or a desktop program, it’s crucial to ensure that user interactions adhere to HIPAA guidelines.
2. Server Interface
The server side of the software is where data processing and business logic reside. Ensuring HIPAA compliance here means safeguarding data and operations against unauthorized access and maintaining data integrity.
3. APIs
Application Programming Interfaces (APIs) act as intermediaries between various software components. It enables seamless communication. Plus, HIPAA compliance extends to how these APIs handle and transmit PHI.
4. Database
The database stores and manages crucial healthcare data. It’s paramount to secure the database environment to prevent breaches or unauthorized data access.
Now, here’s a more detailed step-by-step guide to building HIPAA-compliant applications on AWS:
Sign a Business Associate Agreement (BAA) with AWS
Before you embark on any HIPAA-related activities on AWS, it’s crucial to sign a BAA. This agreement is a legally binding document that outlines how you and AWS will handle, use, and disclose Protected Health Information (PHI).
It ensures that AWS understands its responsibilities and will adhere to HIPAA regulations when managing your data.
Designate Your AWS Account as HIPAA-Compliant
After the BAA is signed, you should mark your AWS account as being HIPAA-compliant. This step is vital because it signals to AWS that you’ll be processing and storing PHI within that account.
In response, AWS will set up mechanisms to alert you if there are any security breaches involving your PHI.
Infrastructure Setup
Setting up your infrastructure with HIPAA compliance in mind means taking several precautions. Ensure that all data is encrypted, both when it’s being transferred and when it’s stored.
Access to this data should be strictly limited to only those who are authorized. It’s also essential to have robust backup and recovery procedures in place, so you can quickly restore data if needed.
Additionally, you should have methods for securely disposing of data and mechanisms to prevent any unauthorized changes or tampering.
Implement HIPAA Policies
Beyond the technical aspects, you need to have organizational policies that align with HIPAA requirements. This involves setting up administrative guidelines that dictate how your organization will handle PHI and remain compliant.
On the technical side, you’ll need to implement specific controls within your AWS infrastructure, ensuring that data is handled correctly and securely at all times.
Regular Monitoring
Compliance isn’t a one-time task. It requires ongoing vigilance. Continuously monitor your AWS environment to ensure that you’re adhering to all HIPAA regulations.
This involves tracking any changes, watching for potential security threats, and ensuring that all data remains secure and compliant.
Therefore, regular reviews and audits can help catch any potential issues before they become significant problems.
The Imperative of HIPAA Compliance
When embarking on the journey to build HIPAA-compliant software on AWS Cloud, it’s not just about meeting the technical requirements.
Equally important is the understanding that HIPAA compliance is not a one-size-fits-all solution. It involves a meticulous evaluation of each component and the entire system to ensure that it aligns with HIPAA guidelines.
So, when implementing HIPAA-compliant software on Amazon Web Services (AWS), there are several crucial factors to keep in mind:
1. Access Control
HIPAA mandates that only authenticated users should access healthcare application resources. AWS uses Identity and Access Management (IAM) to grant specific access to users efficiently.
With IAM, you can create and manage user groups, granting or denying access permissions to AWS resources.
2. Data Backup and Storage
AWS offers a managed solution called AWS Backup. It simplifies the automatic backup of application data for AWS services. This makes the backup process faster and more accessible than traditional methods.
It also ensures compliance by monitoring backup status, current backups, and restored backups. Several AWS services. Such as Elasticache, S3, and RDS, come with built-in backup capabilities.
3. Audit Control
Monitoring and auditing are vital for HIPAA compliance. AWS provides AWS Config, a fully managed service that offers resource inventory. It simplifies auditing, change management, operational troubleshooting, and security analysis.
4. Secure Data Disposal
HIPAA requires the secure deletion of data when it’s no longer needed. AWS allows account owners to configure data retention settings and delete data upon request. It makes sure that unnecessary data is not stored.
5. Encryption and Decryption
AWS offers robust data encryption options. Amazon S3, used for object storage, employs advanced encryption standards like AES-256.
Key Management Service (KMS), a HIPAA-compliant solution, manages encryption keys for various AWS services. KMS uses master keys to encrypt/decrypt PHI data within the application.
Additionally, AWS enables easy encryption of RDS databases and provides SSL encryption for network traffic.
What are the Need for HIPAA Compliance in Healthcare Apps?

HIPAA compliance in healthcare apps is crucial. It ensures that sensitive patient data is protected, meeting both legal standards and maintaining patient trust. In a world prone to data breaches, healthcare apps must prioritize this compliance. But there’s more to know.
1. Entity Consideration
The primary factor revolves around the entity that employs the application. If a healthcare provider or insurer uses the app, they must adhere to HIPAA’s software development requirements.
For example, if you’re developing an app for patient-doctor interactions, HIPAA compliance is imperative. Both doctors and hospitals fall under the category of covered entities, that’s why.
Understanding this aspect necessitates a deep dive into the HIPAA privacy rule. The rule designates two categories of organizations subjected to HIPAA compliance:
- Covered Entities: These encompass healthcare organizations, clearinghouses, providers, and others engaged in electronic financial and administrative transactions, such as electronic billing and fund transfers.
- Business Associates: These entities handle the collection, processing, storage, and sharing of Protected Health Information (PHI) on behalf of covered entities.
2. Data Consideration
The core focus of HIPAA compliance centers on Protected Health Information (PHI). It’s health information capable of identifying an individual, coupled with data generated, disclosed, or utilized during healthcare services like treatment or diagnosis.
Well, PHI comprises two distinct components: medical data and personally identifiable information.
When personally identifiable information is linked to medical data, the resulting information falls under the umbrella of PHI.
An application aiding doctors in diagnosing skin-related conditions by analyzing anonymous photos does not interact with PHI.
However, once the patient’s name or address is introduced into the equation, the information becomes PHI.
3. Software Security Consideration
The final parameter for determining whether a healthcare software development project falls within the purview of HIPAA rules pertains to software security.
This encompasses a range of standards employed to safeguard and control access to electronically Protected Health Information (ePHI).
HIPAA Compliant Software Development in Webisoft
HIPAA Compliant Software Development ensures that software meets the standards set by the Health Insurance Portability and Accountability Act (HIPAA) for safeguarding health information.
On the other hand, Webisoft is a leading software development company, that specializes in creating software that aligns with these HIPAA regulations.
By utilizing Webisoft’s expertise, healthcare organizations can confidently develop digital platforms that are both innovative and compliant. It ensures patient data protection and minimizes legal risks.
Therefore, Webisoft is a go-to partner for secure and compliant healthcare software solutions.
Conclusion
The healthcare industry has undergone a significant transformation. It’s driven by the profound impact of the coronavirus pandemic. This transformation has ushered in a new era of digital healthcare with HIPAA Compliant Software Development.
As a result, there has been a pronounced shift towards emphasizing adherence to healthcare compliance standards.
In this evolving landscape, healthcare organizations are recognizing the importance of compliance. It’s a crucial step forward as we navigate the dynamic terrain of healthcare in the post-pandemic era.
Ready to Elevate Your Healthcare Compliance Efforts? Let Webisoft Lead the Way!
FAQS
What is the significance of data disposal and encryption in maintaining HIPAA compliance?
Proper data disposal and encryption are critical because they prevent data breaches and unauthorized access. HIPAA compliance mandates secure disposal methods and encryption to protect sensitive patient information.
How should backups and data storage be managed in HIPAA-compliant software?
To maintain HIPAA compliance, you must securely store data, and perform regular backups. Also, have a robust plan for data recovery in case of emergencies or data loss. Ensure that your backup procedures meet HIPAA security standards.
What role does automatic logoff play in ensuring HIPAA compliance for healthcare software?
Automatic logoff is essential for security. It terminates user sessions after a period of inactivity, reducing the risk of unauthorized access to patient data.