Healthcare Communication Technology That Fixes Care Gaps
- BLOG
- Digitalization
- October 19, 2025
You feel the difference the moment communication breaks in healthcare, a missed update, a confusing message or a long wait for information. healthcare communication technology steps in to fix these moments by giving you clarity when you need it most.
As care becomes faster, busier and more complex, you need systems that hold everything together. Technology helps your clinicians stay aligned, reduces uncertainty and keeps your journey moving without unnecessary stress.
And as expectations rise, you deserve communication that feels simple, connected and dependable. In this guide, you will understand how the right tools improve care, strengthen your experience and bring more confidence to every step of your healthcare journey.
Contents
- 1 Why Communication Technology Is Essential For Modern Healthcare
- 2 Build smarter healthcare communication solutions with Webisoft.
- 3 Core Categories of Healthcare Communication Technology
- 3.1 1. Digital health records and shared data systems
- 3.2 2. Virtual care and telehealth communication frameworks
- 3.3 3. Patient-facing portals and mobile communication tools
- 3.4 4. Unified communication platforms for clinical teams
- 3.5 5. Remote monitoring systems and connected health devices
- 3.6 6. Integrated communication ecosystems with decision support
- 4 How Communication Technology Improves Clinical Outcomes
- 4.1 Faster decisions grounded in timely information
- 4.2 Higher accuracy through consistent information access
- 4.3 Better long-term management of chronic conditions
- 4.4 Stronger coordination in multi-provider care
- 4.5 Reduction of preventable medical errors
- 4.6 Expanded access that improves outcomes for high-risk groups
- 4.7 Improved preventive care and post-treatment follow-through
- 5 How Communication Technology Improves Patient Experience And Satisfaction
- 5.1 Easier access that removes barriers to care
- 5.2 Faster responses that reduce patient anxiety
- 5.3 Clear visibility into health information
- 5.4 Continuous support between appointments
- 5.5 Reduced time and cost burden for everyday care
- 5.6 Greater involvement in personal health decisions
- 5.7 Care that feels more personal and responsive
- 6 Operational And Administrative Gains Through Communication Modernization
- 6.1 Smoother coordination across departments
- 6.2 Less administrative burden for staff
- 6.3 Clearer visibility into hospital operations
- 6.4 More efficient patient flow through the system
- 6.5 Better use of resources and reduced operational waste
- 6.6 Scalable processes that grow with patient demand
- 6.7 Lower operational costs through automation and streamlining
- 7 Privacy And Security in Healthcare Communication
- 8 Common Risks in Implementing Communication Technology in Healthcare
- 8.1 System failures and technical downtime
- 8.2 Cybersecurity threats and data breaches
- 8.3 Poor interoperability and fragmented data flows
- 8.4 High costs and resource burden for adoption
- 8.5 Staff resistance, lack of training and workflow disruption
- 8.6 Unequal access and digital divide for patients or facilities
- 9 How Webisoft Can Help Implement Effective Healthcare Communication Technology
- 9.1 Rapid prototyping and MVP development for safe experimentation
- 9.2 Custom SaaS and application development tailored to healthcare needs
- 9.3 Legacy system modernization and seamless integration
- 9.4 Scalable, cloud-ready architecture for future growth
- 9.5 Dedicated design and user experience focus to maximize adoption
- 9.6 End-to-end support: from initial consultation to ongoing maintenance
- 9.7 Customizable workflows and privacy-first development
- 10 Build smarter healthcare communication solutions with Webisoft.
- 11 Conclusion
- 12 Frequently Asked Question
Why Communication Technology Is Essential For Modern Healthcare
 Healthcare now runs on rapid coordination and constant information movement. The benefits of communication technology in healthcare become clear as these systems give providers organized, timely and dependable channels that traditional methods cannot maintain.
Healthcare now runs on rapid coordination and constant information movement. The benefits of communication technology in healthcare become clear as these systems give providers organized, timely and dependable channels that traditional methods cannot maintain.
Need for rapid information flow
Time-sensitive updates influence nearly every clinical decision. Healthcare communication technology reduces delays caused by manual processes and disconnected channels, helping teams act quickly and accurately when conditions change.
Care spread across multiple settings
Patients move between specialists, diagnostic services and home-based care. Technology keeps all parties aligned by maintaining continuity across varied environments, reducing gaps when care transitions occur.
Rising complexity of care delivery
Higher patient volumes and staffing pressures make manual coordination unreliable. Digital communication methods reduce dependence on phone calls, paper routing and verbal updates, lowering the chance of avoidable errors.
Importance of real-time awareness
Clinicians need immediate visibility into schedule changes, patient updates and operational shifts.
Findings from the National Library of Medicine study reinforce how real-time communication improves decision-making and overall safety. Communication technology enables fast information sharing, supporting safer decisions and smoother workflows.
Dependence on connected data
Modern healthcare relies on data-supported insights that only function when information flows efficiently. Communication technology provides the structure needed for consistent, connected data movement.
Evolving patient expectations
Patients expect clarity, transparency and timely responses throughout their care journey. Healthcare communication technology supports these expectations without adding unnecessary pressure on clinical or administrative staff.
Build smarter healthcare communication solutions with Webisoft.
Book a consultation to create secure, modern communication systems for healthcare.
Core Categories of Healthcare Communication Technology
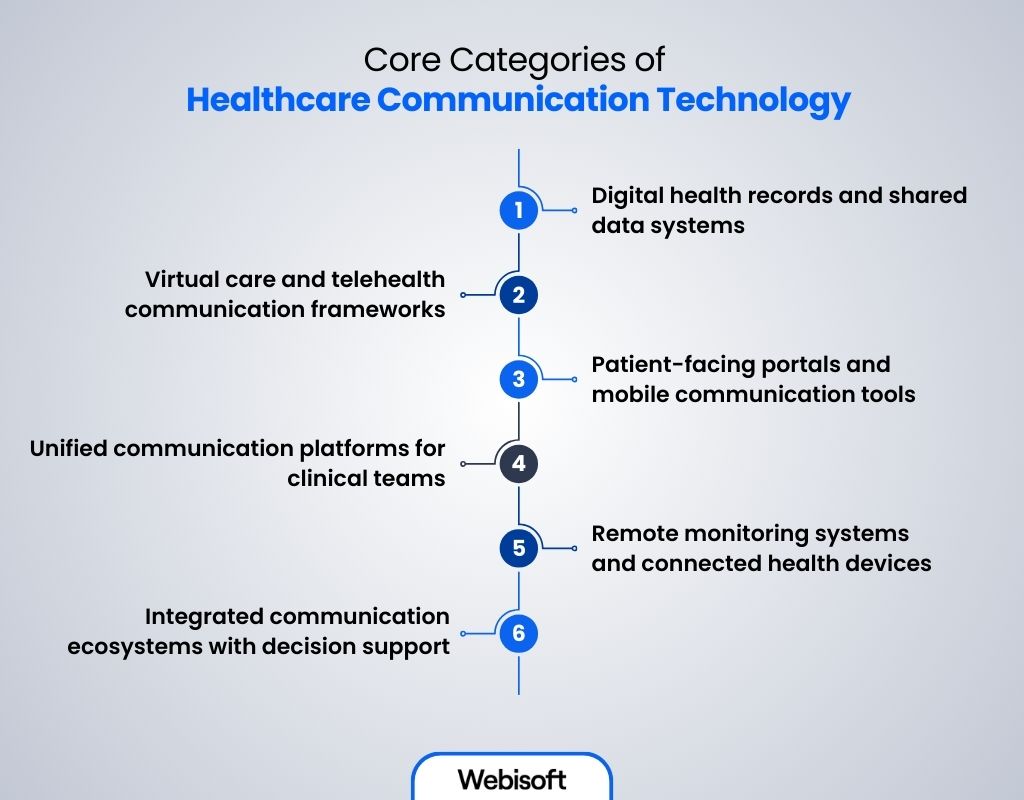 Healthcare communication technology is built on several interconnected categories. Each one shapes how information moves and how teams coordinate, offering technology in healthcare examples that highlight better communication and more reliable care.
Healthcare communication technology is built on several interconnected categories. Each one shapes how information moves and how teams coordinate, offering technology in healthcare examples that highlight better communication and more reliable care.
1. Digital health records and shared data systems
Electronic Health Records form the core of these systems, creating a unified source of truth that supports every clinical decision, strengthened through healthcare software development.
By consolidating medical history, diagnostics and ongoing updates, EHRs ensure providers work from a complete, accurate and current view of a patient’s health. Without this foundation, communication becomes fragmented, decisions lose precision and coordinated care becomes harder to deliver.
Features:
- Structured, continuously updated repositories of medical history and diagnostics
- Multidisciplinary access to unified patient information
- Standardized formats that prevent data loss or interpretation errors
- Permissions, audit logs and access controls for accountability
Benefits:
- Reduces errors caused by outdated or missing information
- Eliminates redundant testing and duplicated workflows
- Improves the speed and precision of clinical decisions
- Strengthens care continuity across departments and providers
Limitations:
- Heavily dependent on accurate input from multiple contributors
- Integration is difficult when organizations use different record systems
- Low face to face communication with the patient
2. Virtual care and telehealth communication frameworks
These frameworks extend communication beyond clinic walls and support safe, high-quality care across distances. They allow providers to maintain relationships with patients, monitor changes and deliver guidance without requiring physical presence.
Features:
- Encrypted video and audio communication channels
- Digital triage tools that direct patients appropriately
- Structured documentation of remote encounters
- Messaging pathways for follow-up clarification
Benefits:
- Expands access to clinicians for remote or mobility-restricted patients
- Enables hybrid care models that blend in-person and virtual support
- Reduces strain on physical facilities by shifting suitable cases online
- Maintains continuity for long-term or follow-up care
Limitations:
- Quality of care can be affected by poor connectivity or device issues
- Not suitable for conditions requiring physical examination or diagnostic tests
3. Patient-facing portals and mobile communication tools
These tools exist to bridge the communication gap between patients and providers by giving individuals direct, convenient access to their own health information. They allow patients to stay informed, take action and engage more actively in their care journey.
Features:
- Real-time access to results, summaries and instructions
- Self-service scheduling, reminders and updates
- Secure messaging for structured communication with clinicians
- Mobile learning resources and task prompts
Benefits:
- Reduces uncertainty by giving patients clarity about their care
- Cuts administrative workload for staff by automating common requests
- Improves adherence through timely and accessible instructions
- Encourages patient involvement and informed decision-making
Limitations:
- Digital literacy varies across patient populations
- Sensitive information must be protected through strong authentication measures
4. Unified communication platforms for clinical teams
These platforms are designed to solve the long-standing coordination problems in healthcare, where dozens of staff members operate in parallel but rely on outdated tools. They ensure that critical information reaches the right professional with the right urgency, without relying on manual routing or guesswork.
Features:
- Real-time messaging, alerts and escalation channels
- Role-based routing to match tasks with responsibilities
- Handoff and shift-transition support
- Visibility into team activity and communication history
Benefits:
- Reduces delays caused by pagers, phone loops or siloed tools
- Prevents miscommunication during emergencies or high-volume periods
- Ensures accountability for message delivery and response
- Improves cross-department coordination
Limitations:
- Without clear role definitions, routing logic can become inconsistent
- Excessive notifications may contribute to alert fatigue
5. Remote monitoring systems and connected health devices
These systems exist to transform continuous patient observation into meaningful communication signals, supported by IoT healthcare software development.
They extend clinical awareness into the patient’s home and allow providers to intervene earlier, manage chronic conditions more effectively and reduce unnecessary in-person visits.
Features:
- Wearables and sensors capturing vitals or condition-specific metrics
- Automated transmission to clinical dashboards
- Threshold-based alerts for concerning patterns
- Longitudinal trend tracking for improved assessment
Benefits:
- Enables proactive intervention before conditions worsen
- Supports safe care for high-risk or chronic patients
- Reduces readmissions through continuous oversight
- Provides clinicians with richer, real-time context
Limitations:
- False alerts can overwhelm clinicians if thresholds are not calibrated
- Patient adherence to wearing or maintaining devices is inconsistent
6. Integrated communication ecosystems with decision support
These ecosystems exist to unify scattered tools, remove workflow fragmentation and embed clinical intelligence directly into communication channels. They combine messaging, analytics and patient context so that providers act on complete information rather than isolated alerts.
Features:
- Unified dashboards showing patient context and team activity
- Automated prioritization and routing based on urgency
- Workflow triggers tied to clinical data
- Integrated guidelines or decision-support insights
Benefits:
- Reduces the cognitive load created by juggling multiple systems
- Ensures communication is meaningful, not just frequent
- Improves efficiency across entire care journeys
- Supports more consistent adherence to clinical standards
Limitations:
- Requires substantial integration effort and technical readiness
- Over-automation can lead to loss of clinical nuance if poorly configured
How Communication Technology Improves Clinical Outcomes
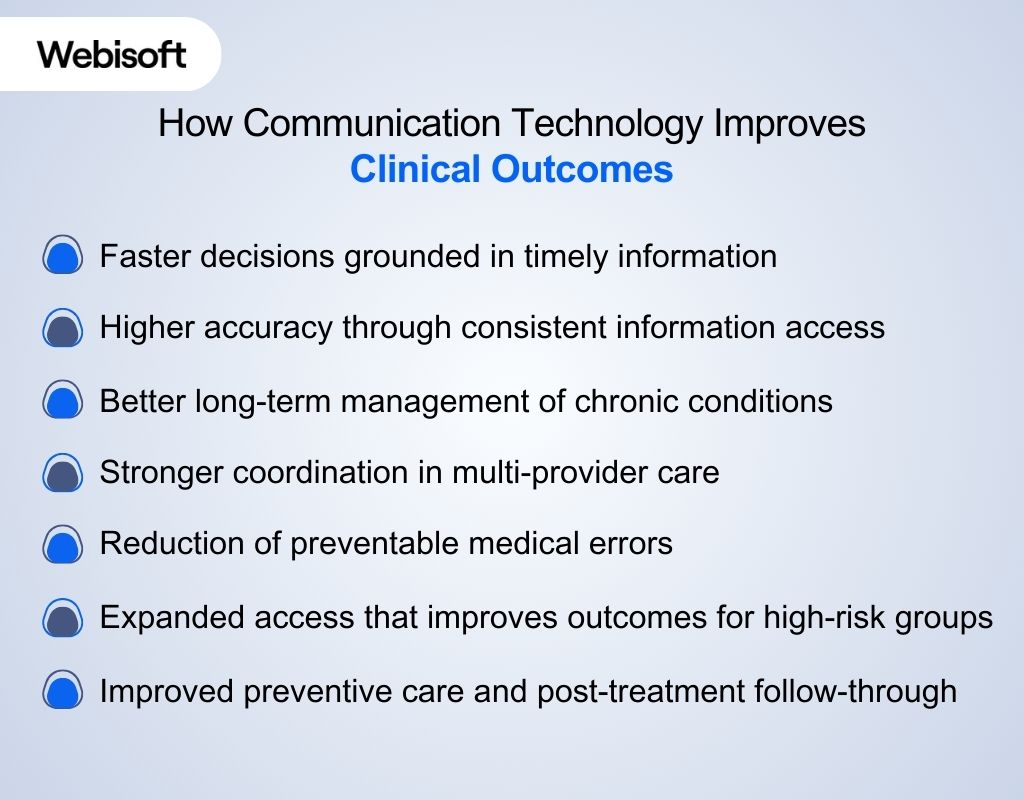 Reliable communication sits at the center of every clinical decision. When information moves accurately and without delay, outcomes improve and complications decrease across all settings. This reflects how does technology improve communication in healthcare by strengthening clarity, speed and consistency in every exchange.
Reliable communication sits at the center of every clinical decision. When information moves accurately and without delay, outcomes improve and complications decrease across all settings. This reflects how does technology improve communication in healthcare by strengthening clarity, speed and consistency in every exchange.
Faster decisions grounded in timely information
- Immediate delivery of critical updates supports rapid clinical action when urgency matters.
- Faster coordination between diagnostic teams and treating clinicians reduces delays in intervention.
- Up-to-date information lowers the risk of complications caused by slow or incomplete communication.
Higher accuracy through consistent information access
- Shared digital information reduces errors linked to handwritten notes or verbal instructions.
- Clinicians work with a complete medical history, reducing the chance of conflicting treatments.
- Consistency across teams eliminates uncertainty during complex or multi-stage care.
Better long-term management of chronic conditions
- Continuous communication supports early detection of worsening symptoms.
- Follow-up instructions and care reminders improve adherence to treatment plans.
- Routine interaction helps stabilize conditions and reduces emergency visits.
Stronger coordination in multi-provider care
- Teams across departments operate with the same clinical context.
- Care transitions become safer when expectations and responsibilities are clearly communicated.
- Treatment planning benefits from shared visibility, especially in complex or high-acuity cases.
Reduction of preventable medical errors
- Structured communication decreases the likelihood of missed information.
- Clear documentation of decisions and updates improves accountability.
- Alerts, acknowledgments and traceable actions help avoid oversights during busy periods.
Expanded access that improves outcomes for high-risk groups
- Patients in remote or underserved regions receive timely care they would otherwise miss.
- Mobility-limited patients have access to evaluation without waiting for in-person visits.
- Timely communication supports early intervention, reducing avoidable deterioration.
Improved preventive care and post-treatment follow-through
- Reminders and instructions help patients complete necessary screenings or follow-up tests.
- Consistent communication after discharge reduces avoidable readmissions.
- Patients receive educational support that improves understanding and long-term health behavior.
How Communication Technology Improves Patient Experience And Satisfaction
 Clinical improvements only tell half the story. Patients feel the difference when communication becomes clear, predictable and supportive. Healthcare communication technology strengthens every touchpoint, helping patients move through their care journey with confidence instead of confusion.
Clinical improvements only tell half the story. Patients feel the difference when communication becomes clear, predictable and supportive. Healthcare communication technology strengthens every touchpoint, helping patients move through their care journey with confidence instead of confusion.
Easier access that removes barriers to care
Video visits, digital check-ins and remote communication give patients access to qualified clinicians without long travel or rigid schedules. People in rural or mobility-limited situations receive timely evaluation and guidance that would otherwise be difficult to obtain.
Faster responses that reduce patient anxiety
Questions no longer wait in phone queues. Messages, updates and alerts reach clinical teams immediately, leading to quicker reassurance and timely action. Patients feel seen and supported when communication does not leave them waiting.
Clear visibility into health information
Patient portals and apps offer immediate access to results, summaries and care instructions. This transparency reduces uncertainty, strengthens trust and helps patients understand what is happening at each step of their care.
Continuous support between appointments
Remote monitoring and digital follow-ups allow patients to stay connected with their care teams even when they are at home. Instructions, reminders and symptom check-ins provide a steady sense of guidance that smooths the recovery or long-term management process.
Reduced time and cost burden for everyday care
Digital communication shortens waiting times, limits unnecessary visits and simplifies routine tasks such as scheduling and clarifying instructions. Patients save time, avoid extra costs and experience a smoother interaction with healthcare services.
Greater involvement in personal health decisions
When information is easy to access and explanations are easier to understand, patients feel more engaged in their care. This empowerment supports better adherence, stronger trust and higher satisfaction with the overall experience.
Care that feels more personal and responsive
Healthcare communication technology allows providers to customize reminders, follow-ups and guidance to the needs of each patient. This sense of personalization makes healthcare feel more human, especially for those managing chronic or long-term conditions.
Ready to strengthen your healthcare communication systems? Connect with the Webisoft team to explore customized digital solutions that fit your clinical and operational goals.
Operational And Administrative Gains Through Communication Modernization
 Better communication not only strengthens clinical care but also transforms the engine that keeps healthcare organizations running. When information moves cleanly behind the scenes, hospitals gain speed, clarity and operational stability that traditional systems cannot deliver.
Better communication not only strengthens clinical care but also transforms the engine that keeps healthcare organizations running. When information moves cleanly behind the scenes, hospitals gain speed, clarity and operational stability that traditional systems cannot deliver.
Smoother coordination across departments
Updates and requests no longer get lost between units. Teams stay synchronized through unified channels that reduce bottlenecks and prevent workflow slowdowns during busy hours.
Less administrative burden for staff
Routine tasks that once consumed hours: scheduling, confirmations, record checks shift into structured digital processes. Staff regain time to focus on higher-value responsibilities rather than repetitive administrative loops.
Clearer visibility into hospital operations
Real-time communication helps leaders understand staffing loads, bed availability and resource use. Decisions become more timely, and facilities operate with fewer blind spots.
More efficient patient flow through the system
From check-in to discharge, communication tools align departments so movement happens without unnecessary pauses. Shorter waiting periods and faster transitions improve overall throughput without adding pressure to staff.
Better use of resources and reduced operational waste
Instant information exchange prevents duplicate paperwork, repeated data entry and unnecessary follow-up calls. Equipment, rooms and personnel are used more strategically when communication is consistent and trackable.
Scalable processes that grow with patient demand
Digital workflows expand far more easily than manual processes. As patient volume increases, communication tools help organizations maintain performance without proportionally increasing administrative workload.
Lower operational costs through automation and streamlining
Automation reduces errors, clarifies accountability and eliminates redundant steps across administrative pathways. Hospitals save time and reduce overhead when communication becomes simpler and more structured.
Privacy And Security in Healthcare Communication
 Digital communication cannot improve care if sensitive patient data is not protected. Secure communication systems are essential to uphold confidentiality, trust and regulatory compliance, which form key pillars of modern healthcare.
Digital communication cannot improve care if sensitive patient data is not protected. Secure communication systems are essential to uphold confidentiality, trust and regulatory compliance, which form key pillars of modern healthcare.
Encrypted and secure communication
Modern platforms use encryption to secure video calls, messages and data transfers so only authorized users can access sensitive health information. This prevents unauthorized access, safeguards electronic personal health information and supports regulatory compliance requirements.
Access control and audit visibility
Role-based access and detailed audit logs help control who sees what by ensuring only permitted staff can view certain records. This traceability helps prevent misuse, supports confidentiality and demonstrates adherence to data-protection regulations.
Secure telehealth practices
Telehealth visits raise privacy concerns when conducted over public networks or shared devices. Secure platforms, consent procedures, private consultation setups and encrypted communication are vital to safely deliver remote care while protecting patient data.
Compliance-aligned communication standards
Regulations such as HIPAA outline strict rules for handling patient information. Secure communication platforms support these standards through controlled access, protected storage and clear data-sharing protocols that reduce legal and ethical risks.
Protection against cyber threats
Healthcare systems face rising exposure to cyberattacks and breaches. Strong security architecture, including encryption, secured networks and regular audits, is essential to prevent unauthorized access and protect patient trust.
Patient control over personal information
Secure communication tools let patients view, manage and authorize access to their records. This transparency builds confidence and supports long-term satisfaction by giving individuals control over their health information.
Common Risks in Implementing Communication Technology in Healthcare
 Integrating new communication tools can unlock powerful benefits, but it also introduces real risks. Healthcare organizations must recognize the risks that can slow adoption or disrupt care to ensure technology becomes an asset rather than a burden.
Integrating new communication tools can unlock powerful benefits, but it also introduces real risks. Healthcare organizations must recognize the risks that can slow adoption or disrupt care to ensure technology becomes an asset rather than a burden.
System failures and technical downtime
When electronic health records or communication platforms crash, critical patient data and messaging can become unavailable. Delays, disrupted workflows, and potential harm escalate if fallback procedures are lacking.
Cybersecurity threats and data breaches
Healthcare systems face an ongoing risk of cyberattacks, ransomware, and unauthorized access, especially when devices and networks are not secured properly. Patient safety and trust suffer when sensitive data is exposed.
Poor interoperability and fragmented data flows
Different systems, EHRs, labs, telehealth, and monitoring often fail to communicate smoothly. This fragmentation can lead to incomplete or inconsistent patient records, undermining coordination and clinical decisions.
High costs and resource burden for adoption
Implementing communication technology demands substantial investment: hardware, software, integration, training, maintenance. Smaller clinics or low-resource settings may struggle to justify or sustain such costs.
Staff resistance, lack of training and workflow disruption
Care teams accustomed to traditional methods may resist change. Without proper training and change management, adoption stalls, leading to underutilization or mistakes in using new systems.
Unequal access and digital divide for patients or facilities
Not all patients or facilities have reliable internet, devices or digital literacy. Over-reliance on digital communication risks leaving behind those in underserved or remote areas, widening care inequities.
How Webisoft Can Help Implement Effective Healthcare Communication Technology
 Healthcare organizations need more than tools; they need a partner who understands communication, workflow and patient expectations. Webisoft steps in with customized product development that turns your vision of modern, secure communication into a dependable reality.
Healthcare organizations need more than tools; they need a partner who understands communication, workflow and patient expectations. Webisoft steps in with customized product development that turns your vision of modern, secure communication into a dependable reality.
Rapid prototyping and MVP development for safe experimentation
With Webisoft’s fast prototyping and MVP services, you can validate your communication concept early: testing workflows, interfaces and user flows with minimal cost and risk. If something needs adjustment, you iterate before committing to full development.
Custom SaaS and application development tailored to healthcare needs
Whether you need a patient-portal, telehealth platform, secure staff messaging tool, or integrated monitoring dashboard, Webisoft builds it from the ground up, customized to the specific compliance, scale and workflow demands of your facility.
Legacy system modernization and seamless integration
If you already have existing systems (EHR, admin software, legacy apps), Webisoft offers legacy transition and integration services, helping migrate or bridge old tools into a unified modern communication ecosystem without painful disruptions.
Scalable, cloud-ready architecture for future growth
Webisoft’s designs use cloud-native and scalable architectures. Ensuring your communication system grows with your organization, whether you start small or expand across multiple clinics or hospitals.
Dedicated design and user experience focus to maximize adoption
Beyond backend code, Webisoft emphasizes UI/UX design and app usability. Increasing the likelihood that both staff and patients will trust, adopt and consistently use the new communication tools. This reduces resistance to change and ensures seamless workflows.
End-to-end support: from initial consultation to ongoing maintenance
Webisoft’s involvement doesn’t stop at launch. From advisory to support, we guide you through planning, deployment, QA/testing, integration, and long-term maintenance. Ensuring that your communication platform remains safe, reliable and updated.
Customizable workflows and privacy-first development
Understanding that healthcare demands strong security and compliance, Webisoft’s custom development lets you embed encryption, access control, audit logging and compliance features from the start, safeguarding patient data and building trust.
Build smarter healthcare communication solutions with Webisoft.
Book a consultation to create secure, modern communication systems for healthcare.
Conclusion
Healthcare communication technology has become the backbone of safer, smoother and more connected care. It closes gaps that once caused delays, strengthens coordination and gives you a clearer, more confident experience across every stage of care.
If you are ready to improve your own communication systems, you deserve a team that can turn complexity into something easy to use. With Webisoft, you get thoughtful, reliable solutions designed to support lasting improvement in your organization.
Frequently Asked Question
Can communication technology support chronic disease management?
Yes. Communication technology strengthens chronic care by enabling remote monitoring, structured symptom reporting and consistent digital follow-ups. These tools help clinicians identify early deterioration, adjust treatment plans proactively, and keep patients safely engaged between in-person visits.
What is unified communication in healthcare?
Unified communication in healthcare brings messaging, alerts, voice, video, and workflow tools together into one platform. It removes fragmented channels, supports real-time coordination and ensures teams stay connected, informed and aligned during routine operations and urgent clinical situations.
Can healthcare communication technology be customized?
Yes. Healthcare communication systems can be customized to match specific workflows, compliance requirements, staffing models and patient needs. Customization improves adoption, strengthens security, supports organizational preferences, and ensures that every feature aligns with real clinical and administrative processes.