Electronic Health Records (EHR) software is a transformative tool in the healthcare sector. It’s a digital leap from the traditional health record systems that often proved to be a labyrinth of paperwork, prone to errors and inefficiency.
EHR software not only digitalizes patient data but makes it readily accessible to healthcare professionals. It resolves the common pain points of traditional systems, such as delayed access to patient records, loss or damage of files, and lack of efficient communication among healthcare providers.
But EHR software is not just about digitizing and organizing health records. It’s about revolutionizing patient care and healthcare administration. It’s an all-in-one solution to the challenges of the conventional system.
In the upcoming sections, we’ll delve deeper into the world of EHR software. We’ll explore how it works, its multiple facets, and its key role in modern healthcare. So, stay tuned for an exciting journey into the future of healthcare management!
Contents
- 1 What is EHR Software?
- 2 Why Should You Consider an Electronic Health Record?
- 3 What is the Difference Between Electronic Health Records (EHRs) and Electronic Medical Records (EMRs)?
- 4 What are the Types of Electronic Health Records (EHRs)?
- 5 Benefits of EHR Software
- 6 Key Features A EHR Software Should Have
- 7 Who are the Main Users of EHRs?
- 8 How does an Electronic Health Records Software Work?
- 9 What Technologies Work in the Back-End of EHR Systems?
- 10 Key Compliance Standards to Keep in Mind When Developing an EHR System
- 10.1 FHIR (Fast Healthcare Interoperability Resources)
- 10.2 HIPAA (Health Insurance Portability and Accountability Act)
- 10.3 DICOM (Digital Imaging and Communications in Medicine)
- 10.4 CCDA (Consolidated Clinical Document Architecture)
- 10.5 SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms)
- 10.6 GDPR (General Data Protection Regulation)
- 11 How to Implement an EHR System
- 12 How to Find Your Ideal EHR System
- 13 How to Select the Best EHR Software Development Company for You
- 14 What are the Services EHR Software Development Companies Offer?
- 15 Why Custom EHR Software Makes Sense?
- 16 Solving the Maze of EHR Implementation: Five Common Issues and Their Solutions
- 17 Top EHR Systems of 2023: A Comparative Overview
- 18 The Future of EHR and Digital Health Trends
- 19 Final Thoughts
What is EHR Software?
EHRs play a pivotal role in modern healthcare by revolutionizing how patient information is managed and utilized.
In an EHR system, each patient has a single record that is continuously updated in real-time. This allows any authorized healthcare provider – be it a physician, nurse, or specialist – to access the most current, comprehensive information about a patient’s health.
Having real-time, reliable data at hand significantly aids in clinical decision-making, promoting more accurate diagnoses, effective treatments, and better patient outcomes. This makes healthcare faster, better, and more convenient for both providers and patients.
In addition, EHRs also enhance the coordination of care. For example, if a patient is referred to a specialist, that specialist can easily access the patient’s EHR to understand their health background, preventing repetition of tests and reducing errors.
A few examples of EHR software include:
- Epic Systems: Known for its comprehensive suite of healthcare software solutions, Epic provides one of the most widely used EHR systems across large healthcare organizations.
- Cerner: Another major player in the field, Cerner’s EHR software, is recognized for its interoperability and extensive health network.
- Allscripts: Providing solutions for both large and small practices, Allscripts EHR is praised for its customizable features and user-friendly interface.
- Meditech: Meditech’s EHR solution is popular among medium to large healthcare facilities for its robust features and integration capabilities.
Why Should You Consider an Electronic Health Record?

There’s a lot to gain from implementing an electronic health record (EHR) system, whether you’re a small practice or a large healthcare organization.
Not only can EHRs boost your cost-effectiveness and patient satisfaction, but they can also significantly improve patient care and reduce medical errors. Essentially, EHRs empower doctors to elevate the standard of care they deliver, enabling them to attend to more patients in less time.
Seamless Health Care Information Connectivity
One of the main reasons healthcare organizations gravitate towards EHRs is their ability to unify patient care services across the system. Information is instantly accessible at any computer terminal, from clinic offices to bedside monitors and nursing stations.
This connectivity extends beyond the primary healthcare system to other providers involved in the patient’s care, facilitating a collaborative approach for optimal patient outcomes.
Reducing Medical Errors
Over time, it’s been observed that EHRs can significantly decrease unintentional medical errors.
EHRs act as an extra layer of safety, cross-checking medications and lab results and alerting clinicians to potential interactions, hazardous values, or urgent health information.
Consequently, with fewer lost or misplaced paper records, the likelihood of inadvertent medical errors drops.
Boosting Efficiency in Health Care Settings
Once your team becomes familiar with EHRs, you’ll notice a marked increase in their productivity and efficiency.
The reason? No more waiting for a paper chart to arrive – clinicians can access comprehensive patient information right where they are.
Other benefits include clearer order entries (no more deciphering illegible handwriting), reduced paperwork, streamlined prescription processes, and the utilization of built-in speech recognition software.
The process of billing also becomes quicker as insurance claim codes can be automatically generated.
Enhancing Patient Care Coordination
In today’s mobile world, patients may frequently move or switch healthcare systems. With EHRs, a patient’s complete medical record can be accessed anywhere, ensuring that valuable health information is never lost.
Improving Patient Outcomes
When a patient’s entire medical history is at the fingertips of their healthcare providers, it naturally leads to better health outcomes.
Clinicians can prevent and treat various conditions more effectively, avoid repeating procedures unnecessarily, and prevent potentially harmful medication interactions. Plus, the patient’s record is always up to date.
Goodbye to Paper Charts
Before the advent of EHRs, storing paper records required large dedicated facilities and significant resources were spent on administrative tasks related to chart maintenance.
With EHRs, all records are safely and conveniently stored digitally, accessible anytime and anywhere. Illegibility and lost information become things of the past, thanks to computerized storage and EHR servers.
Financial Savings
For healthcare systems seeking to economize, EHRs are an excellent solution. Saving time means saving money, as staff can work more efficiently and see more patients daily.
Plus, the expenses of maintaining storage facilities and managing paper chart retrieval are eliminated.
Moreover, government incentives, such as the 2009 stimulus package linked to the Health Information Technology for Economic and Clinical Health Act, provide reimbursements for EHR implementation. Even Medicaid now mandates the use of EHRs for reimbursement.
What is the Difference Between Electronic Health Records (EHRs) and Electronic Medical Records (EMRs)?

In short, while EHRs and EMRs both provide digital medical records, there is a key distinction between the two. EMRs are like digital versions of a patient’s chart in a single practice. They contain the medical and treatment history of patients within one office.
However, EHRs provide a broader, more holistic view of a patient’s health. They encompass a patient’s complete health profile and can be shared across different healthcare settings.
Now, to better understand, let’s dig deeper into the distinction between EHRs and EMRs.
Electronic Medical Records (EMRs) are essentially digital versions of the traditional patient chart within a doctor’s office. They keep track of data over time, flag check-ups or screenings that are due, and track the patient’s health parameters.
However, the scope of EMRs is limited to the practice where the patient’s data is recorded. In other words, EMRs don’t travel well outside the practice.
On the other hand, Electronic Health Records (EHRs) are designed to be a more comprehensive record of the patient’s overall health. They go beyond the data collected in a healthcare provider’s office and include information from all clinicians involved in a patient’s care.
The data in EHRs is designed to be shared with other providers, so they provide a holistic, long-term view of patient care.
Here’s a comparison table for a clearer understanding:
| Parameters | EMRs | EHRs |
| Scope | Limited to the practice where patient data was recorded | Broad view across healthcare providers |
| Patient Data | Contains medical and treatment history within one office | Contains a comprehensive health profile |
| Data Sharing | Difficult to share data outside the practice | Designed for easy data sharing |
| Objective | Digital version of a traditional chart, aids in diagnosis and treatment | Designed to streamline overall patient health management |
| Portability | Not portable, resides within the confines of one practice | Portable and can be accessed across different healthcare settings |
In a nutshell, while EMRs are a significant leap forward from paper records, EHRs take it to the next level by providing a comprehensive, portable health record that can be accessed across various healthcare settings. This allows for improved patient care, increased efficiency, and better health outcomes.
What are the Types of Electronic Health Records (EHRs)?
EHR systems can be classified into two primary types:
Physician-Hosted Electronic Health Records
Physician-hosted EHR systems store patient data on servers within the physicians’ or organizations’ own infrastructure. Traditional in nature, these solutions come with substantial costs for hardware and software procurement, along with on-site installation.
This type of EHR platform provides robust control over patient data but also faces occasional downtime during system updates and patches, requiring temporary system shutdowns.
However, these systems are a viable choice for larger organizations with the revenue to cover the overhead costs of purchase and maintenance.
Example: Epic Systems is a well-known provider of physician-hosted EHR systems, catering predominantly to large hospitals and healthcare networks due to its comprehensive suite of applications.
Remotely-Hosted Electronic Health Records
Remotely-hosted EHR systems house patient data on the vendor’s servers, significantly alleviating the hardware and software management burden.
These technologically advanced systems are a boon for medium-sized practices aiming to avoid hefty immediate software purchase costs.
These systems offer the benefit of access from any location with internet connectivity and come with automatic updates and upgrades managed by the vendor. The system typically falls into three categories:
Subsidized
Perfect for small practices, this model involves a partnership with a third-party entity that subsidizes the EHR server’s cost. But, physicians surrender data ownership in this model, leading to potential future ownership issues.
Example: Community Health Systems offers a subsidized EHR program where the company subsidizes the cost of implementing and maintaining the EHR software for associated physicians and practices.
Dedicated
In this model, physicians engage in a contract with the vendor to locate the EHR at a specific site. Even though physicians lack data control, they are informed of its location.
Example: Allscripts is a prominent player offering dedicated EHR solutions, providing a mix of on-premise and hosted solutions depending on the client’s needs.
Cloud
As mentioned earlier, cloud-based EHRs are popular worldwide. Patient data is stored on a server managed by the vendor, allowing around-the-clock access for physicians and medical staff. Practices can opt for a monthly or yearly payment plan instead of an upfront cost.
Example: Athenahealth is a prime example of a cloud-based EHR system provider, offering a subscription-based model with extensive scalability and flexibility.
Benefits of EHR Software
Merging digital technology with modern medicine, EHR systems bring a revolution in care delivery. The seamless flow of information they provide introduces numerous advantages.
Increasing Patient Care
With EHRs, providers get quick access to comprehensive and legible patient records, regardless of their location. This access enables more coordinated and efficient patient care, improving overall care quality.
Boosting Patient Engagement
EHR software encourages patient participation by making healthcare more accessible. Features like telehealth and secure communication channels give patients the flexibility to interact with their healthcare providers without physically visiting clinics.
E-prescribing ensures prescriptions are prepared even before the patient leaves the provider’s office, adding to the convenience.
Enhancing Care Coordination
EHRs effectively reduce care fragmentation by improving coordination. They organize patient health information and allow real-time sharing among all authorized care providers.
This universal access to the latest patient information is crucial, especially for patients consulting multiple specialists, undergoing emergency treatments, or transitioning between care settings.
By eliminating the chance of information mismatch, EHRs reduce medical errors and unnecessary tests.
Improved Diagnostics and Health Outcomes
EHRs streamline the collection, analysis, and sharing of patient information. This empowers healthcare providers with complete, accurate data, boosting their diagnostic capabilities, reducing errors, and enhancing patient care quality. The result? Improved health outcomes.
Efficiency Boost and Cost Reduction for Practices
EHRs contribute significantly to enhancing practice efficiency and reducing costs. Some of the ways they do this include:
- Lowering transcription costs – Comprehensive charting and coding can be done with a few clicks, even before the patient leaves the clinic.
- Reducing expenses related to physical records – No more costs for paper chart storage or refiling.
- Minimizing medical errors – EHRs give better access to patient data and provide error prevention alerts.
- Streamlining practice management – EHRs offer integrated scheduling systems that link appointments directly to progress notes, automate coding, and handle claims.
To be noted, EHRs are not just about digitizing health records. They are about transforming healthcare delivery, improving patient experiences, and optimizing practice operations.
Key Features A EHR Software Should Have
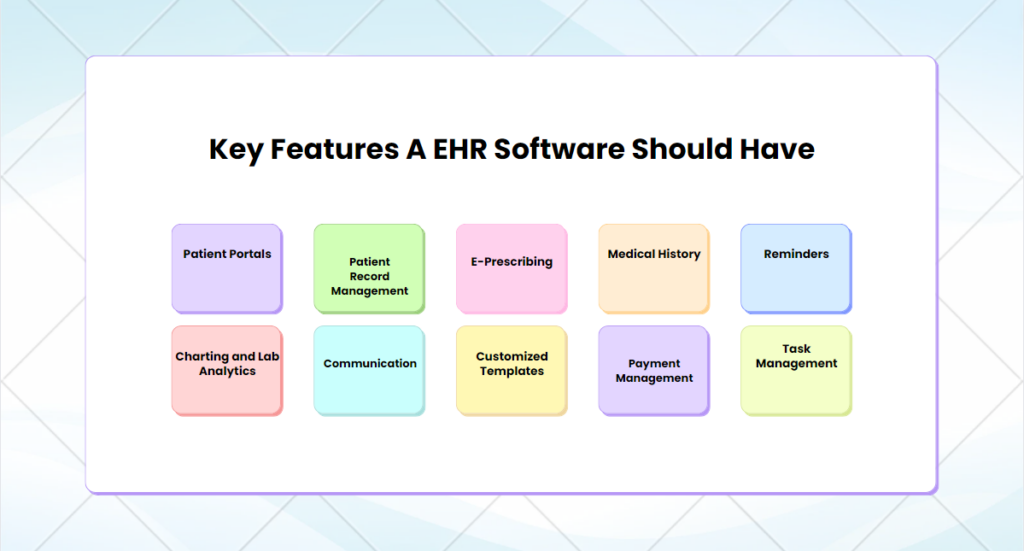
EHRs come packed with a variety of features designed to streamline patient care and healthcare administration. Here are some key features:
Patient Portals
Patient portals stand as a critical component in the landscape of modern EHR systems. These portals serve as a digital gateway for patients, creating a space for comprehensive health management.
These portals facilitate secure access to personal health records, enabling patients to stay informed about their medical status and history. By offering transparency, these systems can boost patients’ trust in their healthcare providers and the treatments administered.
Additionally, these portals allow for efficient appointment scheduling, streamlining the traditional process of booking appointments through phone calls or in-person visits. This convenience significantly enhances patients’ experiences, making healthcare more accessible and patient-friendly.
Patient Record Management
Efficient patient record management is at the core of EHRs. This feature allows secure storage, rapid retrieval, and effective management of patient health records.
It minimizes the risk of lost or misplaced records, reduces administrative work, and enables healthcare providers to easily track a patient’s health progress over time.
E-Prescribing
E-Prescribing is another notable feature of EHRs. It enables healthcare providers to send prescriptions directly to pharmacies electronically, reducing paperwork, minimizing prescription errors, and increasing efficiency.
This feature also aids in medication management, alerting providers about potential drug interactions or allergies.
Medical History
A comprehensive medical history repository is a vital component of EHRs. It allows providers to view a patient’s past diagnoses, treatments, allergies, immunizations, and more, all in one place.
This holistic view of a patient’s health journey enables providers to make more accurate diagnoses and informed treatment decisions.
Reminders
Reminders in EHR systems ensure important health actions are not forgotten. Whether it’s an appointment, medication, preventive care, or follow-up, reminders help both patients and providers stay on top of necessary health tasks.
Charting and Lab Analytics
Charting and lab analytics in EHRs help visualize patient health data, chart trends, and analyze lab results. This feature supports clinical decision-making by providing visual insights into patient health status and progress, making it easier to detect abnormalities and monitor treatment effectiveness.
Communication
Communication is integral to successful healthcare delivery, and EHRs facilitate this effectively. Whether it’s interdepartmental communication among doctors and nurses, or interaction between patients and healthcare providers, EHRs enable streamlined, efficient, and secure communication.
Customized Templates
Customized templates in EHRs allow healthcare providers to tailor the EHR interface to their specific needs and workflows. Whether it’s a custom input form or a specialized report format, these templates can greatly improve data input efficiency and information retrieval.
Payment Management
Payment management features in EHRs simplify the billing and payment processes. They automate invoice generation, track patient payments, and manage insurance claims. This leads to smoother financial operations, reduced billing errors, and improved revenue cycle management.
Task Management
Task management tools in EHR systems help streamline workflows and delegate tasks efficiently. They assist in keeping track of pending tasks, managing staff schedules, and monitoring task completion, enhancing productivity within the healthcare setting.
Each of these features plays a massive role in improving patient care, enhancing workflow efficiency, and boosting the overall productivity of healthcare settings. By leveraging these features, healthcare providers can reap the full benefits of EHR systems.
Who are the Main Users of EHRs?
Electronic health records are securely stored on servers or within the cloud, ensuring that only authorized individuals can access sensitive patient data. Enhanced security measures such as biometric and two-step access systems further safeguard against data misuse.
The primary users of EHRs typically include healthcare providers and patients themselves.
Healthcare Providers
Originally conceived as a digital alternative to cumbersome paper charts, EHRs have become an indispensable tool for healthcare providers. These professionals use EHRs to access patients’ historical health data, medication records, and radiology reports.
EHRs enable physicians to issue new prescriptions, refill existing ones, order and review lab or radiology studies, and communicate directly with patients.
In addition, EHRs serve as a platform for collaboration, enabling healthcare providers involved in a patient’s care to exchange vital information. Today, a majority of physicians rely heavily on EHRs for documenting patient interactions.
Beyond this, billing teams can manage invoicing and payments directly through the EHR, negating the need for physical paperwork.
Patients
While EHRs may have initially been developed with healthcare providers in mind, patients stand to gain significantly from these systems.
EHRs serve as a direct line of communication with physicians, enabling patients to ask questions about health issues or seek clarification on medication instructions.
Depending on the system, patients can also access their past visit summaries, view laboratory results as soon as they become available, request medication refills, and settle bills with ease.
Certain platforms even provide healthcare educational resources, empowering patients to take a more active role in managing their health.
How does an Electronic Health Records Software Work?
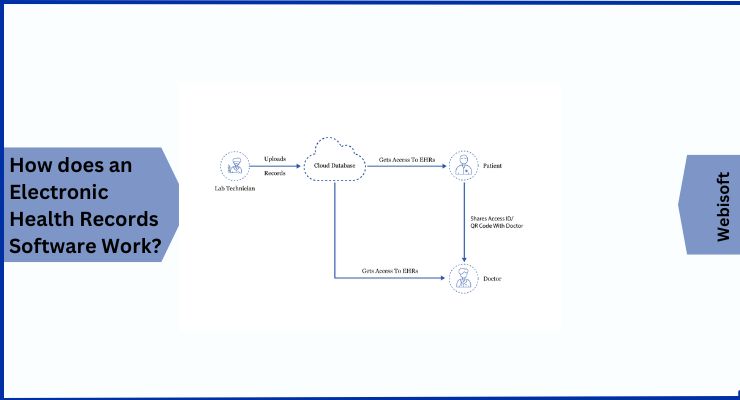
While the specifics can vary given that different systems often come with different features, we’re going to break down how a basic, patient-centric, cloud-hosted EHR system works, using a relatable example.
Let’s imagine you have diabetes and your doctor advises you to get your blood sugar levels checked.
Once your test is done, your reports get uploaded onto a secure cloud database, which is accessible only to you. To share these reports with your doctor, you provide them an access ID or QR code. This allows your doctor to access your records.
What’s cool about this is that you can set a time limit for how long the doctor can access these records. This could be a few hours or a few days depending on what you’re comfortable with. During this window, your doctor can add various elements to the records like:
- Prescriptions
- Notes
- Lab results
- Future appointments
- Payment updates
- Charts
- Treatment routines, etc.
This way, your medical data remains secure and only authorized individuals can make updates.
And let’s say down the line, you decide to change your doctor. You won’t have to deal with the hassle of transferring your medical records from your previous doctor. They’re all already updated and ready to go. You can easily share them with any new doctor and revoke access from your previous one.
Now that we’ve covered the basics of how EHR software works, let’s dive into the technology stack that’s used to build such a system.
What Technologies Work in the Back-End of EHR Systems?
Planning to create your own custom EHR software? You’ll need a robust technology stack to do so. This stack is typically divided into front-end and back-end components that communicate through Application Programming Interfaces (APIs).
Let’s take a deep dive into the technology behind it.
1. Front-End Development
The front-end is the interface that users interact with. It includes the design and layout of the EHR software.
- Web: For web-based platforms, HTML5 is often used as the markup language to structure and present content on the web, and JavaScript is used for interactive elements. JavaScript frameworks like Angular and React are popular for their ability to create responsive and dynamic user interfaces.
- iOS: For iOS platforms, Swift 5 and Objective C are commonly used. Swift is known for its speed and safety, while Objective C maintains legacy code within Apple. Development usually takes place on the latest version of macOS, with XCode 11 or AppCode being the integrated development environment (IDE) of choice. The iOS SDK and Cocoa Touch offer a range of tools and interfaces for developing iOS applications.
- Android: Kotlin and Java are often used for Android platforms. Kotlin is more modern and has null safety, while Java is used in large legacy systems. The development operating system could either be macOS or Ubuntu. The latest Android Studio is typically used as the IDE, while the latest Android SDK provides the APIs necessary to develop Android applications.
2. Back-End Development
The back-end is the server-side of the software where data is stored and manipulated. This is what allows the front-end to function and is critical for an EHR system.
- Programming Language: Languages like Ruby, Elixir, Python, PHP, and Java are often used. These languages are robust, versatile, and widely supported, making them ideal for back-end development.
- Database (DB) Server: The database server hosts the database and responds to queries. PostgreSQL, MySQL, Oracle Database, and DB2 are some of the widely-used options due to their performance and scalability.
- Web Server: A web server serves the requested HTML pages or files to the client. NGINX, Apache, and Node.js are some of the most commonly used due to their efficiency, flexibility, and speed.
- Web Frameworks: Web frameworks like Ruby On Rails, Phoenix, and Django help streamline web application development by offering libraries for database access, session management, and code reuse.
- Cloud Server: Cloud servers like Amazon Web Services (AWS), Microsoft Azure, or Google Cloud provide on-demand cloud computing platforms and APIs to individuals, companies, and governments, on a metered pay-as-you-go basis.
- Application Programming Interfaces (APIs):APIs connect the front-end and back-end functionalities and facilitate integration with third-party tools.
- Payment Gateways: Payment gateways like Stripe, PayPal, and Braintree enable healthcare organizations to receive direct payments from patients. This simplifies the payment process and ensures smooth financial transactions.
- Video Conferencing APIs: APIs like Twilio, Agora, TenHands API, or AuraLink API allow healthcare providers to conduct virtual consultations by integrating video conferencing functionality into the EHR software.
- Scheduling APIs: APIs like YellowSchedule or PostHook API provide calendar integration that displays doctor availability and enables appointment booking.
- Chat APIs: APIs like MessageBird Chat API or Banckle Chat API enable real-time messaging within the EHR software, promoting easy communication between patients and providers.
In conclusion, developing a reliable and effective EHR system requires a blend of the right technologies. By understanding and selecting the appropriate technology stack, one can ensure the development of an EHR system that is secure, user-friendly, and efficient.
Key Compliance Standards to Keep in Mind When Developing an EHR System
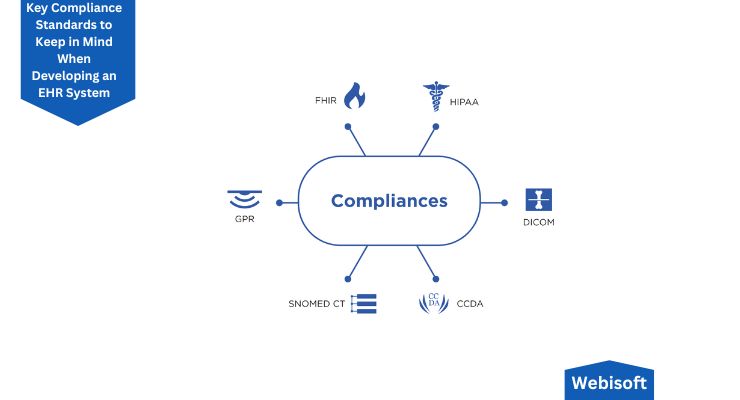
Creating an Electronic Health Record (EHR) system requires not just a robust tech stack but also adherence to certain compliances and standards. These ensure the privacy and security of patient data, seamless exchange of healthcare information, and overall interoperability.
Let’s check out the six key compliances and standards for EHR software.
FHIR (Fast Healthcare Interoperability Resources)
FHIR is a widely adopted standard for the exchange of digital health information. It defines the elements, data formats, and an application programming interface (API) for exchanging electronic health records.
With the increasing reliance on EHRs, FHIR ensures these records can be interpreted and used by diverse healthcare systems.
The primary goal of FHIR is to standardize the exchange of patient data, enabling healthcare providers, even those using different software, to share and utilize this data.
HIPAA (Health Insurance Portability and Accountability Act)
HIPAA is a critical compliance standard that establishes rules for the security and privacy of patient information.
While EHRs bring several benefits to both healthcare providers and patients, they can potentially jeopardize patient privacy and data security. HIPAA compliance ensures the advantages of EHRs are reaped without compromising patient privacy.
It includes numerous rules for EHR software development, specifically addressing the collection, processing, and storage of patient data.
DICOM (Digital Imaging and Communications in Medicine)
DICOM is a globally accepted standard for the communication and management of medical imaging data. It covers five primary application areas: network image management, network image interpretation management, network print management, imaging procedure management, and offline storage media management.
CCDA (Consolidated Clinical Document Architecture)
CCDA is a markup standard that streamlines the creation of templates and documents for medical information. This documentation aims to reduce ambiguity and inconsistency in medical documentation.
It encompasses a library of clinical document architecture template standards and serves as a guide for the development of various electronic clinical documents or EHRs.
CCDA provides a common architecture, coding, semantic framework, and markup language for communicating patient health data, administrative healthcare data, and patient population data.
SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms)
SNOMED CT is a comprehensive and computer-processable collection of medical terms that facilitates consistent clinical reporting and documentation. This is known as the most comprehensive and multilingual clinical terminology globally.
It offers codes, terms, synonyms, and definitions and is considered an essential standard for interoperability in the United States’ healthcare IT systems.
GDPR (General Data Protection Regulation)
The GDPR is a European Union law regulating digital data privacy and protection. It mandates strict policies for the collection, processing, and safeguarding of personal data.
It’s applicable to the healthcare industry as providers must ensure maximum protection of patient information and swiftly correct or delete data upon request.
So, it’s important to remember that the rules and regulations for EHR software development can vary by country or region. Always ensure that you are aware of and adhere to the specific compliances and standards relevant to your geographic location before initiating the EHR software development process.
How to Implement an EHR System
So, now, are you looking to implement Electronic Health Records (EHR) software successfully? The path to implementation can seem daunting, but fret not! With the right approach and a step-by-step plan, you can achieve it with relative ease. Let’s take a journey through the process.
1. Assemble an Implementation Dream Team
Kick off your EHR implementation by forming a dynamic team. This group should consist of key stakeholders, including doctors, nurses, receptionists, and administrative staff. There are three key roles to focus on:
- Project Manager: Think of them as the conductor of your EHR implementation orchestra. They cooperate with your chosen EHR software development company/vendor, keep track of deadlines, manage daily issues, and ensure the project runs smoothly.
- Head Physician: This individual is your EHR champion, who ensures effective communication between all parties involved. They play a crucial role in bridging the gap between technical, administrative, and front-end users.
- Head Super User: A super user is someone who understands your internal processes like the back of their hand. Their job is to configure the software, create templates, design workflows, and troubleshoot front-end user issues.
2. Set Up The Software
This step involves close collaboration between your IT department and the EHR software development company. You’ll need to list the features you require, such as custom templates, medication management, billing management, and more.
Additionally, it’s essential to identify and ensure compliance with legal standards according to your geographic area, like HIPAA, CCDA, GDPR, etc.
3. Check Hardware Requirements
Determining the hardware requirements is crucial to the seamless implementation of your EHR software. These requirements can vary depending on your organization’s unique needs.
Whether you need to install printers in every office or equip your doctors with portable devices, this step can save you significant time and money.
4. Data Migration
With your new system in place, it’s time to transfer all your data from the previous record-keeping system to your new EHR.
This process requires meticulous planning, categorization of data, and efficient execution, possibly involving additional temporary staff if your data volume is significant.
5. Optimize Workflows
This step might feel unnecessary but trust me, it’s not! Streamlining your workflows before the final system launch helps everyone know their tasks and avoids post-launch chaos.
This proactive approach ensures that tasks are done in the right order, with fewer mistakes and confusion.
6. Decide on a Launch Approach
There are two common launch strategies for EHRs:
- The Immediate/Big Bang Approach
- The Incremental Approach
The former involves switching all users to the new system on the same day, while the latter implements the system gradually, either feature by feature or department by department.
Both have their merits, so you’ll need to decide which suits your organization best.
7. Train Your Staff
The last step, but by no means the least, is staff training. Ensuring your team members can effectively use the system is crucial to the successful implementation of your EHR software. Create a detailed training plan and schedule sessions to address each issue systematically. You can better plan for future support and help by identifying weak areas early.
Successfully implementing an EHR system can seem overwhelming, but with a planned approach and a dedicated team, you’ll soon realize this technology’s numerous benefits to your organization.
How to Find Your Ideal EHR System
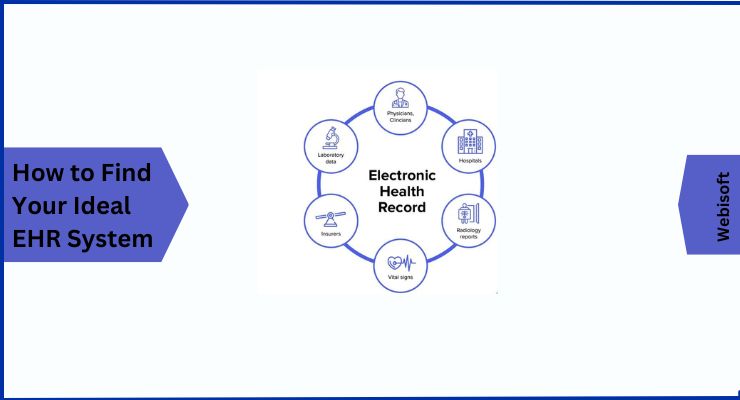
If you’re aiming to amplify patient outcomes and enhance the overall efficiency of your practice, the right EHR system can be an invaluable asset. It can simplify documentation, save money, and keep your processes modern and streamlined.
It’s essential to remember that every medical practice is distinct, each with its unique needs and demands from an EHR. So, when you start scouting for the perfect EHR, it’s crucial to have a clear picture of what you’re seeking in terms of features and the kind of EHR software.
Let’s talk about some key features you should weigh when choosing top-tier EHR software:
Billing
An ideal EHR system should simplify billing and claims processing. This not only results in quicker payments but also boosts revenue.
Electronic Prescriptions
This feature empowers providers to send clear, accurate, and understandable prescriptions electronically straight to a pharmacy, right from the point of care.
Patient Portal
This is a handy way for patients to interact with their healthcare providers and play a more proactive role in their healthcare. They can easily access results from outpatient laboratory and radiology tests, for instance.
Scheduling
This feature ensures your practice stays busy and efficient by providing an easy way for patients to schedule appointments online or through their patient portal. It can also send out reminders for appointments.
Telehealth
This is a secure, HIPAA-compliant, and user-friendly way to bridge the gap between providers and patients when an in-office visit may be challenging due to time, distance, or other constraints.
Remember, your EHR system should work for you, making your practice smoother and more efficient. It’s all about finding the one that ticks all your boxes!
How to Select the Best EHR Software Development Company for You
Choosing the right EHR software can transform your practice, boosting patient outcomes and operational efficiency. But remember, every practice is unique, so your EHR software should cater to your specific needs.
Here’s a five-step guide to help you find your ideal EHR software development partner:
1. Connect with Your Network
Begin by reaching out to colleagues or contacts who have experience with EHR software development companies. Their insights and reviews can be invaluable and help you filter out the companies that don’t quite hit the mark.
Take your research online, too – reading reviews can shed more light on potential partners.
2. Investigate Work Profiles
Visit the websites of the companies that caught your attention.
Check out their previous work – this will give you a glimpse into their quality of work and whether their style aligns with your needs.
Peek at their social media profiles and blogs to gauge their level of activity and get a sense of their work process.
3. Narrow Down Your Options
Based on your findings, create a shortlist of potential companies. Detail the specific EHR services you’d like from them and note their contact information. It’s like preparing a shopping list before heading to the store!
4. Open a Line of Communication
Now’s the time to get in touch with the shortlisted companies and arrange meetings. When you sit down with them, gauge their level of dedication. Discuss key aspects such as price structure, project timeline, and the team’s expertise and experience.
5. Make Your Choice
After your meetings, weigh up the pros and cons of each company. Take into account their cost, team experience, and overall compatibility with your needs.
Once you’ve analyzed all this, you’re ready to make your choice and hire your ideal EHR software development company.
What are the Services EHR Software Development Companies Offer?
EHR software development companies cater to a broad range of needs, but there are five fundamental services you’ll find in their portfolios:
Custom EHR Software Development
These companies can craft an EHR solution to your exact specifications, with a focus on security features and robust operation. You get a system designed just for you, keeping your specific needs in mind.
EHR Implementation and Integration
Seamless integration of EHR software into your current system or coupling it with third-party systems like document management software or cloud-based billing is no small task. That’s where these experts come into play, ensuring a smooth transition and efficient operation.
EHR Mobile App Development
The mobility of data is a critical aspect of modern healthcare. EHR companies offer the development of mobile applications that provide ease of access and use for healthcare providers.
Support and Maintenance
With continuous support and regular maintenance services, these companies are there to help whenever you face any software issues. This includes resolving bugs and carrying out necessary upgrades, ensuring your software runs optimally.
Compliances
To ensure patient data privacy and security, your EHR software needs to adhere to certain compliances and standards for electronic information exchange. EHR companies can help ensure that your software meets all necessary standards, respecting the rules of your geographical area.
All this might have you considering a custom EHR solution, right? Let’s delve into why a customized EHR software can be your best bet.
Why Custom EHR Software Makes Sense?
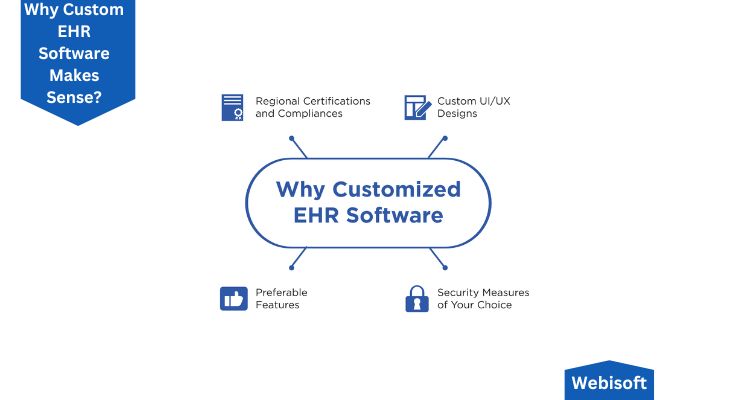
Every healthcare institute is different, each with unique needs that may not be met by off-the-shelf EHR software. This is where custom EHR software comes into the picture. Here are four compelling reasons to go custom:
Regional Certifications and Compliances
With custom software, you can meet the specific compliances and certifications of your area without compromising on features. Off-the-shelf solutions may not always meet these standards.
Enhanced Security Measures
Custom EHR solutions let you build in your desired security measures, ensuring your patients’ data is secure. You can even integrate technologies like blockchain for enhanced security.
Custom UI/UX Designs
With custom software, the user interface can be designed to your liking, ensuring ease of use, smooth workflows, and a pleasing aesthetic. This way, the software becomes easy to navigate and highly organized.
Preferable Features
A custom solution enables you to incorporate only the features you need and ignore those you don’t. For instance, if you already have a separate cloud-based billing system, you can integrate it with your EHR software, saving both time and money.
Choosing a custom EHR software development service allows you to get exactly what you need, contributing to more effective and efficient healthcare practice.
Solving the Maze of EHR Implementation: Five Common Issues and Their Solutions
Embarking on the journey of EHR implementation? It’s not always a smooth ride. You might encounter some bumps and bends along the way, but knowing how to tackle them can make your path less arduous. Here, I’m outlining the five most common challenges healthcare providers face during EHR implementation, along with some tips to overcome them.
1. The Cost Conundrum
Admittedly, the initial cost of EHR integration can be a bit daunting, and it’s one of the key reasons many healthcare organizations hit the brakes. However, look at it as a valuable investment. With an appropriately implemented EHR system, you’ll notice a rise in revenue, cost reduction, and efficiency boosts. So, in the long run, it’s worth every penny.
2. Taming the Usability Beast
Sometimes, EHR and EMR systems can be more of a hindrance than a help, mainly due to their lack of usability. Poor design, inappropriate alerts, and complicated navigation can cause errors, frustration, and a slowdown in productivity.
According to David Lareau, CEO of Medicomp Systems, the antidote to this issue lies in leveraging AI technologies.
These can optimize workflows, making patient data more accessible, ultimately improving patient care and minimizing frustrations.
3. Data Privacy Concerns
Data privacy is a critical concern for healthcare professionals. Some worry that constantly updating EHR systems and migrating patient data to new systems can be counterproductive.
However, the risks of not transitioning to digital solutions far outweigh the challenges. EHRs are equipped with robust security features, protecting sensitive information from potential breaches.
Ensure to ask your software developer about ONC and HIPAA certifications and standard security protocols like audit trails, protected passwords, and data encryptions.
4. Conquering Data Migration Mountains
Transitioning from an old system to a new one is a significant hurdle, particularly when it comes to preserving data integrity.
Experts like Robert Havasy from the Personal Connected Health Alliance and Teri Burley from Leidos Health suggest teaming up with a third-party abstraction partner. This collaboration can help plan, manage, and implement a comprehensive, long-term data integration strategy effectively.
5. Ensuring EHR Interoperability
EHR interoperability, the ability of various programs to share information and work together, is essential. If your EHR system isn’t capable of seamless communication with other systems, you’ll miss out on a lot of the benefits of electronic records.
To overcome this, ask your software provider about features that enhance network communication, such as cloud-based systems, blockchain, and application programming interfaces (APIs).
Remember, EHR implementation is a significant step, but the right approach and the right partner can make this journey rewarding. Stay informed, ask the right questions, and you’ll find that the challenges aren’t insurmountable after all.
Top EHR Systems of 2023: A Comparative Overview
Picking out the right Electronic Health Record (EHR) system can be a daunting task, with a myriad of options at your disposal. However, don’t worry. We’ve compiled a list of the top EHR systems of 2023 that cater to different requirements, making it easier for you to select the best fit for your healthcare organization.
1. DrChrono
If you’re on the lookout for an EHR system that seamlessly integrates with iOS mobile devices, DrChrono is your go-to choice. It’s intuitive, user-friendly, and designed to facilitate quick and efficient access to patient data, perfect for healthcare providers on the move.
2. Practice Fusion

Aimed at independent practices, Practice Fusion stands out with its comprehensive features, ease of use, and affordable pricing structure. It’s the ideal choice if you are an independent practitioner seeking a comprehensive EHR solution that won’t break the bank.
3. Kareo Clinical
When it comes to small medical practices grappling with medical billing, Kareo Clinical is a frontrunner. Its straightforward yet powerful billing features help streamline your revenue cycle management process, leading to fewer errors and faster payments.
4. Netsmart myUnity
For long-term care practices, Netsmart myUnity is an excellent choice. It’s specifically designed to address the complex needs and workflows of long-term care, making it a reliable partner in providing quality patient care.
5. AdvancedMD
Catering to large group practices, AdvancedMD offers a robust set of features aimed at managing vast patient data, appointments, and billing, making it an effective solution for large healthcare settings looking to streamline their workflows.
6. NextGen
If your focus is on improving population health outcomes, NextGen can be your perfect ally. Its advanced analytics tools allow for detailed health outcome tracking and management, supporting better healthcare delivery.
7. Athenahealth
Ideal for large healthcare organizations, Athenahealth offers an array of features to handle complex and high-volume data, ensuring smooth operations and improved patient care in larger healthcare settings.
8. eClinicalWorks
As telehealth gains momentum, eClinicalWorks proves to be a leader in this space. Its top-tier telehealth technology facilitates remote consultations, making healthcare more accessible, especially during times when in-person visits might not be feasible.
9. Valant
For behavioral health practices, Valant is an optimal choice. It’s uniquely designed to address the specific requirements of this sector, contributing to improved patient management and treatment outcomes.
10. Cerner
Finally, for organizations operating across multiple sites, Cerner emerges as the top choice. Its robust, interoperable system seamlessly connects diverse healthcare settings, ensuring comprehensive and integrated care delivery.
There you have it, the cream of the crop for EHR systems in 2023. By understanding the unique strengths of each system, you can align them with your specific needs and choose the one that serves your healthcare organization best.
The Future of EHR and Digital Health Trends
In 2016, the global market for Electronic Health Records was valued at a healthy $20.55 billion, but it’s expected to soar to $33.41 billion by 2025. Major tech giants are playing a significant role in this growth, carving out their space in the flourishing digital health market.
The Projections: EHR Systems Usage in the US
There’s no denying the importance of EHRs and digital health tools in today’s medical landscape. Let’s look at how Google’s parent company, Alphabet, is stepping into this space.
They’re leveraging their cloud platform to address the tricky issue of EHR interoperability, positioning themselves to secure valuable partnerships with health systems.
In 2018, they introduced Google Cloud for Healthcare, a platform designed to aid clinicians in gathering and accessing patients’ health data.
Their Cloud Healthcare API simplifies data exchange between healthcare applications while still complying with industry-specific privacy and security regulations. The ultimate aim? Turning EHRs into powerful decision-support tools.
In 2019, Apple, too, decided to get in on the EHR action. They forged a deal to incorporate data from Allscripts’ EHR into their Apple Health Records platform.
Considering that Allscripts ranks as the fifth largest EHR vendor in the US, according to Business Insider Intelligence, this partnership positions Apple to increase its hospital market penetration substantially.
Amazon isn’t sitting on the sidelines, either. Through Amazon Web Services (AWS), they’re gathering data from sources such as EHRs to aid healthcare providers in their decision-making process and predict potential risks to patients.
Interestingly, research from Business Insider Intelligence suggests that 62% of healthcare organizations view Amazon’s potential move positively, signaling a favorable shift for the medical industry.
Meanwhile, other big tech companies, particularly those in transportation and patient convenience, are contributing to the growth of the EHR market. Take Uber, for example.
They’ve tapped into the non emergency medical transport opportunity by enabling provider organizations using Cerner EHRs to arrange Uber rides for their patients. Quite an exciting time for EHRs and digital health, wouldn’t you agree?
Final Thoughts
In the world of healthcare, the demand for Electronic Health Records (EHR) Software is reaching new heights. Its introduction has ushered in a new era of efficiency in record management, making it a must-have for many hospitals and healthcare organizations.
It’s not hard to see why so many are keen to implement EHR software in their systems – the promise of optimized results and boosted productivity is truly compelling.
However, adopting an EHR system is a significant move that brings a whole host of considerations. It’s dramatically improving how patient data is managed, laying the foundation for a more streamlined, efficient, and patient-centric healthcare experience.
Now, how about taking that crucial next step toward your digital transformation journey? At Webisoft, we’re experts in providing tailored EHR Software services, designed with your specific needs and goals in mind.
Why wait? Let’s start the conversation about how we can revolutionize your record management today.

