In the ever-evolving world of healthcare, Electronic Health Record (EHR) interoperability has emerged as a vital component in enhancing patient care, streamlining processes, and ensuring seamless communication among various healthcare entities.
EHR interoperability, while promising, is a journey filled with challenges. However, these problems can be overcome with strategic thinking, careful planning, and a holistic approach.
By weaving together standards, security, collaboration, education, technology, regulations, and patient engagement, we can create a healthcare system that’s efficient but also compassionate and patient-centric.
The future of healthcare is interconnected, and with the right steps, we can ensure that this interconnection leads to better health outcomes for all. But what exactly does Electronic Health Record interoperability entail, and why is it so crucial in modern healthcare?
This comprehensive article will delve into the intricacies of EHR interoperability, the challenges, and the strategies to overcome them.
Contents
- 1 What Does Interoperability in Healthcare Imply?
- 2 What Are Healthcare Interoperability Challenges?
- 3 How to Overcome These Challenges?
- 4 How to Proceed With the EHR Interoperability Implementation?
- 5 What Are the Benefits of EHR Interoperability?
- 5.1 1. Improved Patient Care: A Personalized Approach
- 5.2 2. Cost Savings: Efficiency that Translates to Dollars
- 5.3 3. Enhanced Collaboration: Coordinated Care for Comprehensive Healing
- 5.4 4. Increased Efficiency: More Time for What Matters Most
- 5.5 5. Empowered Patients: Taking Control of Health
- 5.6 6. Compliance and Reporting: Simplified Yet Robust
- 5.7 7. Innovation and Research: A Gateway to the Future
- 6 Conclusion
What Does Interoperability in Healthcare Imply?
Interoperability in healthcare is a multifaceted concept that goes beyond mere technical integration. It’s a dynamic synergy that combines various elements to create a seamless healthcare experience.
Let’s delve into what this truly means.
Data Sharing In Interoperabiity
- Unifying Patient Records: Different providers hold different pieces of patient information. Interoperability unifies these records.
- Timely Access: Emergencies require immediate information. Interoperability ensures timely access to vital data.
- Reducing Redundancy: Duplicate tests and procedures are wasteful. Interoperability helps in reducing such redundancy.
- Enhancing Research: Shared data can fuel medical research. Interoperability makes this sharing possible.
- Global Reach: Diseases know no borders. Interoperability enables global data sharing for better healthcare.
Enhanced Collaboration
- Coordinated Care: Multiple specialists often treat patients. Interoperability ensures coordinated care among all.
- Real-time Communication: Instant communication can save lives. Interoperability enables real-time collaboration.
- Shared Decision Making: Patients, doctors, and nurses all have roles. Interoperability fosters shared decision-making.
- Breaking Silos: Departments often work in silos. Interoperability breaks these barriers to holistic care.
- Community Engagement: Healthcare involves communities. Interoperability brings communities into collaborative healthcare efforts.
Patient-Centered Care For Promoting Interoperability
- Personalized Treatment Plans: Every patient is unique. Interoperability enables truly personalized treatment plans.
- Empowering Patients: Knowledge is power. Interoperability gives patients access to their data.
- Remote Monitoring: Chronic conditions need constant monitoring. Interoperability enables remote patient monitoring.
- Health Education: Educated patients make better choices. Interoperability can deliver personalized health education.
- Family Involvement: Families are part of care. Interoperability includes them in the care process.
EHR Technological Integration
- Software Communication: Different software must talk. Interoperability ensures they communicate effectively.
- Device Connectivity: Medical devices generate vital data. Interoperability connects these devices for integrated care.
- Scalability: Healthcare needs to keep growing. Interoperability ensures that technology can scale with needs.
- Security: Patient data is sensitive. Interoperability must ensure robust security measures.
- Compliance: Regulations guide healthcare. Interoperability must align with legal and regulatory compliance.
Financial Considerations
- Cost Efficiency: Wasteful practices cost money. Interoperability helps cut unnecessary expenses.
- Billing Accuracy: Accurate billing builds trust. Interoperability ensures that bills reflect actual care.
- Insurance Collaboration: Insurance is part of healthcare. Interoperability streamlines insurance processes.
- Investment Planning: Technology needs investment. Interoperability guides wise technology investment decisions.
Social and Ethical Aspects
- Ethical Data Use: Ethics guide data use. Interoperability must align with ethical guidelines.
- Cultural Sensitivity: Different cultures have different needs. Interoperability respects and accommodates cultural diversity.
- Community Trust: Trust is the foundation. Interoperability builds community trust through transparency and accountability.
Interoperability in healthcare is not just a technical term; it’s a philosophy that embodies the essence of integrated, patient-centered, efficient, and ethical healthcare.
From data sharing to enhanced collaboration, patient empowerment to technological integration, and financial considerations to social and ethical aspects, Interoperability weaves these threads into a cohesive fabric.
It’s about creating a connected ecosystem where patient information doesn’t just flow; it dances to the rhythm of empathy, efficiency, and excellence. That’s what Interoperability in healthcare truly implies.
What Are Healthcare Interoperability Challenges?

The concept of EHR (Electronic Health Records) interoperability is indeed promising. Yet, it’s not without its challenges. Let’s delve into some of the most common obstacles:
1. Technical Challenges
Healthcare interoperability is not a straightforward journey. Technical, organizational, and cultural challenges abound.
Incompatible systems, resistance to change, and privacy concerns are just the tip of the iceberg. Yet, the promise of EHR interoperability is too great to ignore.
- Incompatible Systems: Different EHR systems may clash. Communication barriers arise from incompatibility. Seamless data exchange becomes difficult. Patients’ care might suffer as a result. Solutions require careful planning and execution.
- Data Standardization: Standardized data formats are often lacking. Information exchange becomes a hurdle. Healthcare providers struggle to communicate. Patient care can be compromised. The industry needs unified standards.
- Security Concerns: Patient data must remain secure. Ensuring privacy is complex. Breaches can have severe consequences. Trust in healthcare providers is paramount. Security measures must be robust and adaptable.
2. Organizational Challenges
Solutions require collaboration, innovation, and a commitment to patient care.
Standardization, security, and a willingness to embrace change are essential. The path may be challenging, but the destination is worth the effort.
- Resistance to Change: Healthcare providers may resist change. New technologies can be intimidating. Existing workflows may be disrupted. Progress becomes slow and cumbersome. Change management strategies are essential.
- Cost Constraints: Implementing interoperable systems is costly. Smaller healthcare providers may struggle. Budget limitations can hinder progress. Quality care should not be compromised. Financial planning and support are key.
- Legal and Regulatory Compliance: Legal landscapes are complex. Regulatory compliance is challenging. Sensitive patient data adds complexity. Missteps can lead to legal issues. Expertise in healthcare law is vital.
3. Cultural Challenges
Healthcare providers, regulators, and patients must come together. A shared vision, clear communication, and a focus on quality care can overcome the obstacles.
The future of healthcare is interconnected, and Interoperability is the key.
- Lack of Collaboration: Collaboration is often lacking. Information sharing becomes hindered. Patient care may suffer as a result. A culture of openness is needed. Healthcare providers must work together.
- Patient Privacy Concerns: Patient privacy is delicate. Information sharing needs balance. Privacy concerns can hinder progress. Patients must trust their providers. Ethical considerations are paramount.
The challenges are real, but so are the solutions. With determination, expertise, and a patient-centered approach, healthcare interoperability can move from concept to reality. The benefits are clear, and the time to act is now.
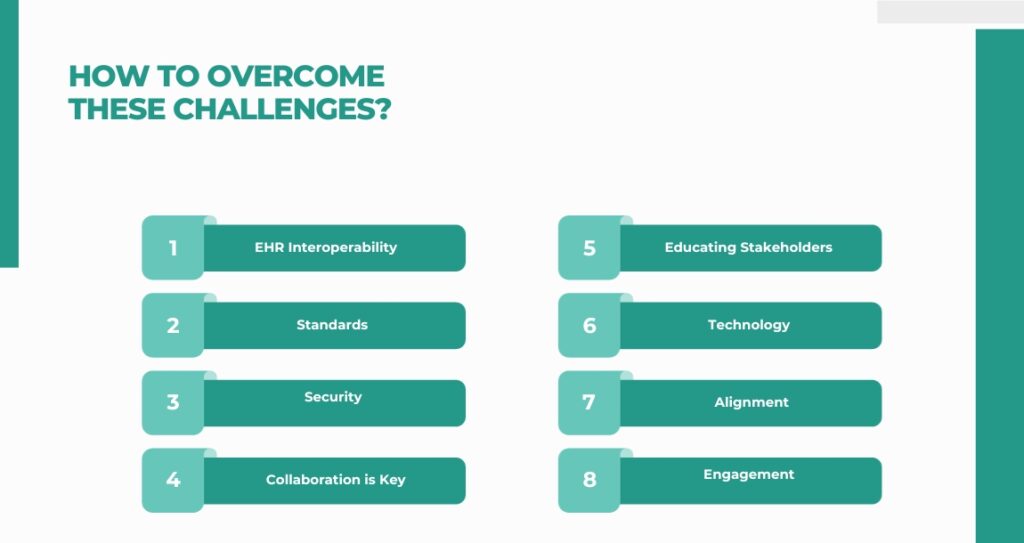
How to Overcome These Challenges?
The world of healthcare is evolving rapidly, and one of the most promising advancements is EHR (Electronic Health Record) interoperability.
But as with any significant technological shift, there are challenges to overcome. Let’s dive deep into understanding these challenges and how to navigate them.
1. Understanding EHR Interoperability
At its core, EHR interoperability standards ensure that different information technology systems and software applications in healthcare can communicate effectively.
It’s about creating a connected ecosystem where patient information flows seamlessly, regardless of platform or location.
This seamless flow ensures healthcare providers have the right information at the right time, leading to better patient outcomes.
2. The Need for Standards
One of the foundational steps toward achieving Interoperability is the adoption of standardized data formats and protocols.
By understanding and choosing the right standards, healthcare providers can ensure smoother information exchange. Regular monitoring and evolving with these standards are crucial to stay updated.
3. Security: A Paramount Concern
Given the sensitive nature of medical data, security is of utmost importance. This means assessing unique security needs, implementing robust protocols, and planning for disaster recovery.
Regular security audits and managing patient consent for data sharing are also integral parts of the security framework.
4. Collaboration is Key
For EHR interoperability to be truly effective, fostering collaboration among stakeholders is essential.
Building trust, encouraging open communication, and recognizing collaborative efforts can go a long way in ensuring that different systems and teams work together harmoniously.
5. Educating Stakeholders
Education plays a crucial role in the successful implementation of EHR interoperability.
This involves identifying learning needs, developing tailored educational content, and ensuring continuous education to keep up with the evolving landscape.
6. Leveraging the Right Technology
Technology is the backbone of EHR interoperability. This involves choosing interoperable technology, integrating different systems effectively, and ensuring regular performance monitoring. As technology evolves, regular upgrades are necessary to stay current.
7. Regulatory Alignment
Laws and regulations guide the realm of EHR interoperability benefits. Understanding these legal requirements, implementing compliance measures, and engaging legal expertise is essential to ensure the system aligns with all legal mandates.
8. Patient Engagement: The Heart of Healthcare
Last but certainly not least, patients are at the heart of healthcare. Educating them, addressing their concerns, involving them in decisions, and respecting their choices are all crucial aspects of EHR interoperability.
How to Proceed With the EHR Interoperability Implementation?
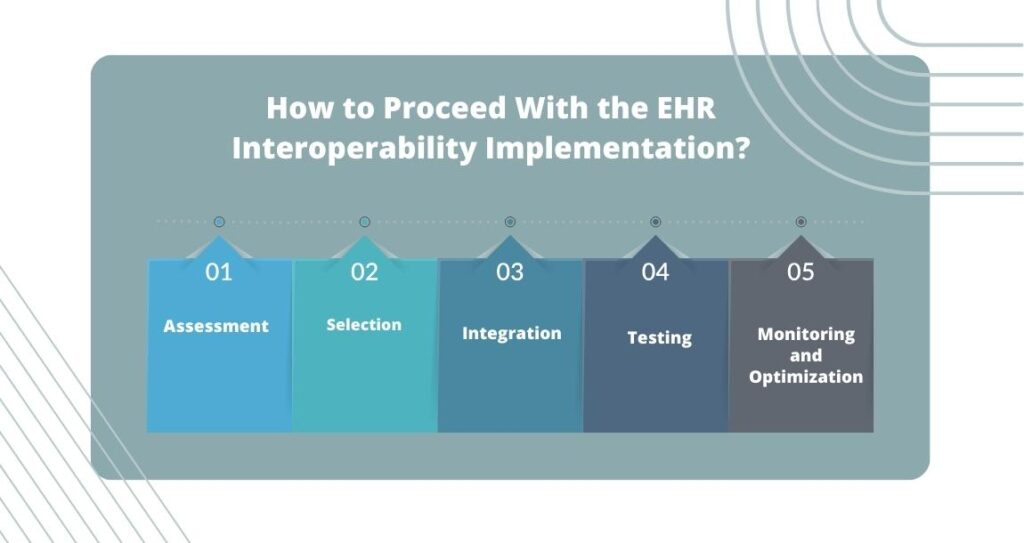
Implementing EHR (Electronic Health Records) Interoperability is like piecing together a complex puzzle. It’s a multifaceted task that requires careful planning, precise execution, and continuous monitoring. Let’s explore the journey together.
1. Assessment: The Foundation of Success
The first step is understanding the current state of your systems. You need to know what’s working and what’s not, identify the gaps, and define your interoperability goals.
Engaging all relevant stakeholders ensures everyone’s on the same page, and collaboration becomes the key to success. Creating a clear roadmap guides the process, setting the stage for what’s to come.
2. Selection: Choosing the Right Tools
Selection is about choosing the right technologies and platforms that align with your needs and objectives. It’s like picking the right tools for a job.
You need to consider functionality, scalability, cost, and, most importantly, security. Consulting with experts can guide your selection.
3. Integration: Making Everything Work Together
Integration is where the magic happens. It’s about ensuring the selected systems can communicate and work together seamlessly.
Addressing compatibility issues, ensuring effective communication, and collaborating with technology vendors are all part of this crucial phase. It’s like building a bridge between different islands, ensuring everything is connected and functioning as a cohesive whole.
4. Testing: Ensuring Robustness
Testing is where you put everything to the test. It’s about simulating real-world conditions, identifying glitches or weaknesses, and including end-users.
Their feedback is essential, as the user experience must be positive and efficient. Iterating as needed ensures the system is robust and ready for the real world.
5. Monitoring and Optimization: Continuous Improvement
The journey doesn’t end with implementation. Continuous monitoring and optimization are vital. Keeping an eye on system performance, making necessary adjustments, evaluating user feedback, and ensuring compliance with regulations are ongoing tasks.
It’s about continuous improvement, enhancing performance, and maintaining the system’s longevity and trustworthiness. Implementing EHR interoperability is indeed a journey, not a destination.
Each step builds on the previous one, from assessment to optimization, leading to a system that can transform healthcare. Challenges will undoubtedly arise but can be overcome with careful planning, collaboration, and a patient-centered approach.
The EHR interoperability benefits are profound, and the effort is more than worthwhile. The future of healthcare is interconnected. By following this structured and thoughtful process, healthcare providers can unlock the potential of interoperable systems.
What Are the Benefits of EHR Interoperability?
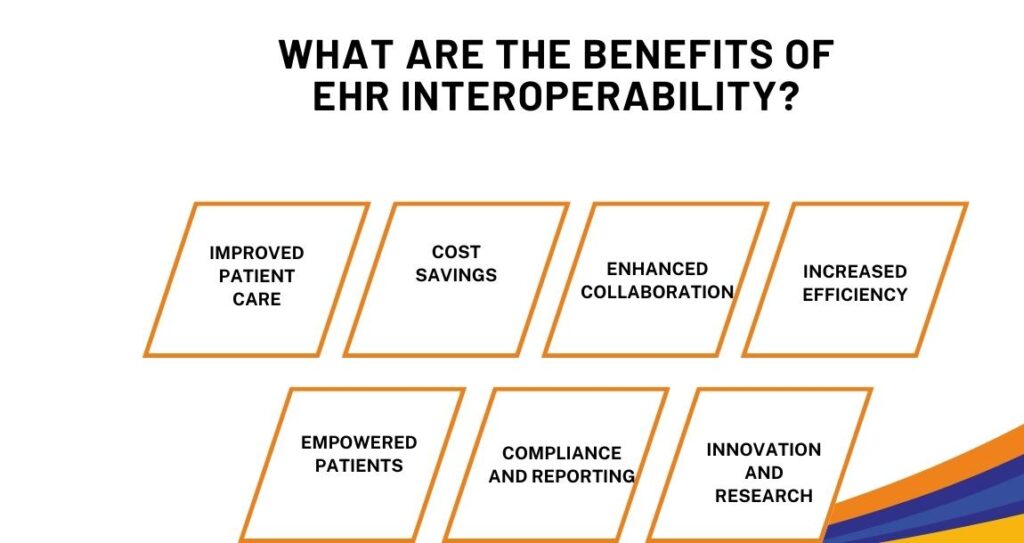
EHR interoperability is more than a buzzword in the healthcare industry; it’s a transformative force reshaping healthcare delivery.
Let’s explore the myriad benefits that EHR interoperability brings to the table.
1. Improved Patient Care: A Personalized Approach
One of the most profound impacts of EHR interoperability solutions is the enhancement of patient care. Comprehensive patient information becomes readily accessible to healthcare providers.
No longer do doctors have to make decisions based on fragmented information. A complete medical history, including previous diagnoses, treatments, and even allergies, is available at the click of a button.
This comprehensive view enables healthcare providers to offer more accurate, personalized care. Patients receive treatments tailored to their unique needs and medical history. The result is better care and care that feels personal and considerate.
2. Cost Savings: Efficiency that Translates to Dollars
The healthcare industry is no stranger to costs; any opportunity to save without compromising care quality is welcome. EHR interoperability offers this opportunity.
By streamlining processes and reducing duplication, it cuts down administrative burdens. Paperwork that once took hours can now be completed in minutes.
Repeated tests due to lost or inaccessible results have become a thing of the past. These efficiencies add up, leading to significant cost savings.
Hospitals save, insurers save, and ultimately, patients save. It’s a win-win situation that makes healthcare better and more affordable.
3. Enhanced Collaboration: Coordinated Care for Comprehensive Healing
Healthcare is rarely about one doctor or one treatment. It’s a collaborative effort involving specialists, nurses, pharmacists, and family members. EHR interoperability fosters this collaboration by creating a platform for storing and sharing information.
A patient’s primary care physician can coordinate with specialists, therapists, and others involved in the patient’s care. Information flows seamlessly, ensuring that everyone is on the same page.
This coordinated approach leads to more holistic care, where every aspect of the patient’s health is considered and addressed. It’s about treating the person, not just the disease.
4. Increased Efficiency: More Time for What Matters Most
In the hustle and bustle of healthcare, efficiency is paramount. EHR interoperability brings this efficiency by automating processes and enabling seamless information flow.
Tasks that once consumed valuable time are now automated. Information that was once buried in files is now readily accessible. Healthcare providers find themselves freed from administrative shackles.
They can spend more time listening, understanding, diagnosing, treating, and comforting. Efficiency in processes translates to richness in care. It’s about technology making healthcare more human.
5. Empowered Patients: Taking Control of Health
EHR interoperability is not just about healthcare providers but also patients. Patients become more than passive care recipients with access to their medical records.
They can better understand their health, make informed decisions, and share information with healthcare providers. This empowerment builds trust, fosters engagement, and enhances satisfaction. It’s about patients feeling in control of their health and care journey.
6. Compliance and Reporting: Simplified Yet Robust
Regulations and reporting requirements are part and parcel of healthcare. EHR interoperability simplifies these aspects by providing a transparent, accurate, and easily accessible patient care record.
Compliance becomes less cumbersome, and reporting becomes more accurate. It’s about meeting legal obligations without the stress and strain that often accompany them.
7. Innovation and Research: A Gateway to the Future
Finally, EHR interoperability opens doors to innovation and research. Researchers can uncover patterns, make discoveries, and even pioneer new treatments.
It’s a gateway to the future of healthcare, where data-driven insights lead to breakthroughs that save lives and enhance well-being. EHR interoperability is not just a technological shift; it’s a cultural shift.
It’s about embracing a new way of delivering healthcare – one that’s more connected, efficient, collaborative, patient-centered, and innovative. It’s about recognizing that in the complexity and diversity of healthcare, connectivity is not a luxury but a necessity.
That’s the promise and the power of EHR interoperability. It’s a promise worth pursuing and a power worth unleashing.
Conclusion
EHR interoperability is not just a technological trend; it’s a fundamental shift in how healthcare is delivered and managed. While achieving full EHR interoperability may be challenging, the rewards are substantial.
By understanding the complexities, recognizing the obstacles, and implementing strategic solutions, healthcare providers can unlock the true potential of EHR interoperability.
At Webisoft, we are committed to helping you navigate this journey, offering cutting-edge solutions tailored to your unique needs.Contact our health-tech experts today to explore how we can transform your healthcare delivery through EHR interoperability.